What is a retinal vein occlusion?
All tissues in the body need a blood supply to function as the blood provides the cells with oxygen and sugar which they need to survive. The blood going to the tissues from the heart travels in blood vessels called arteries. These then divide up into much smaller blood vessels called capillaries where the oxygen and sugar is given to the cells and the waste products such as carbon dioxide are given back to the blood. These capillaries then join up to form larger blood vessels called veins which return the blood to the heart.
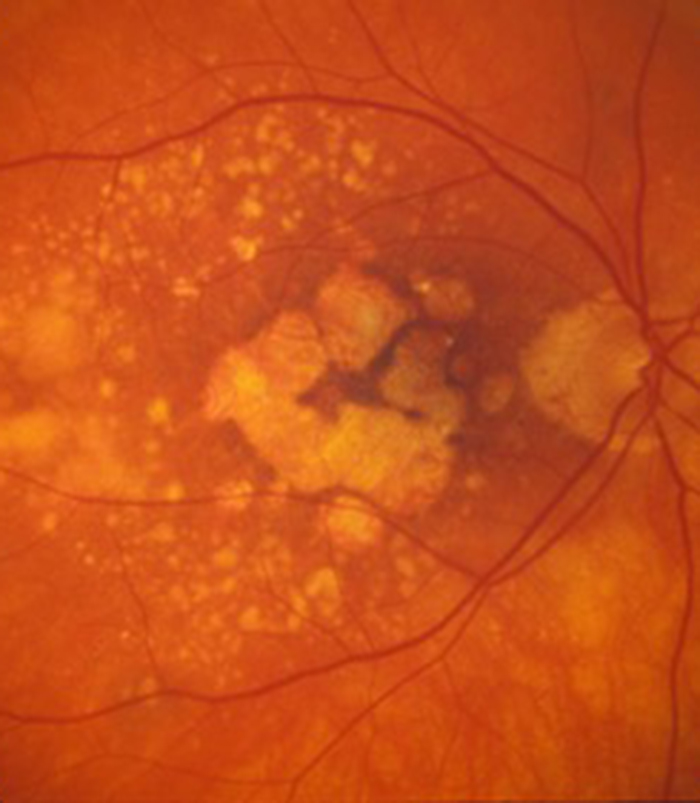
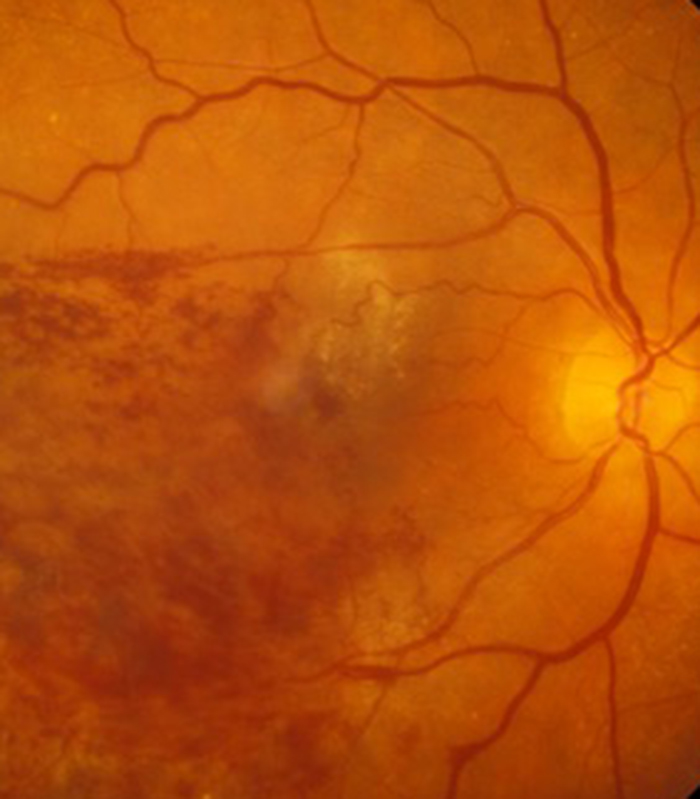
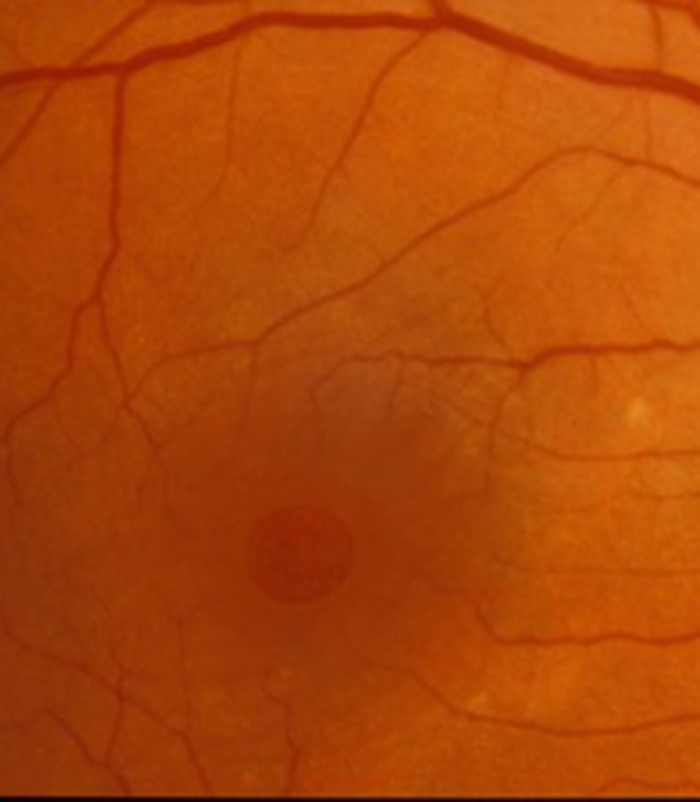
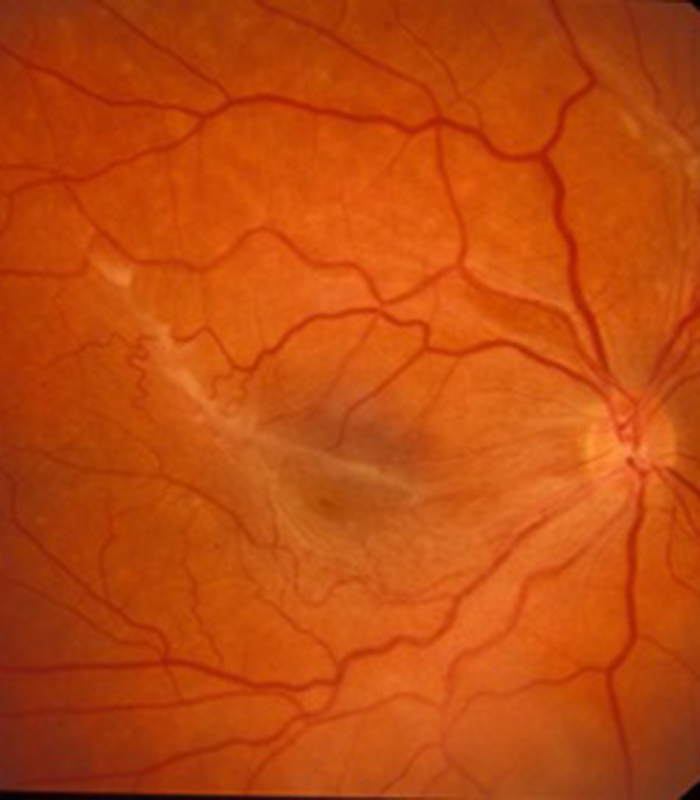
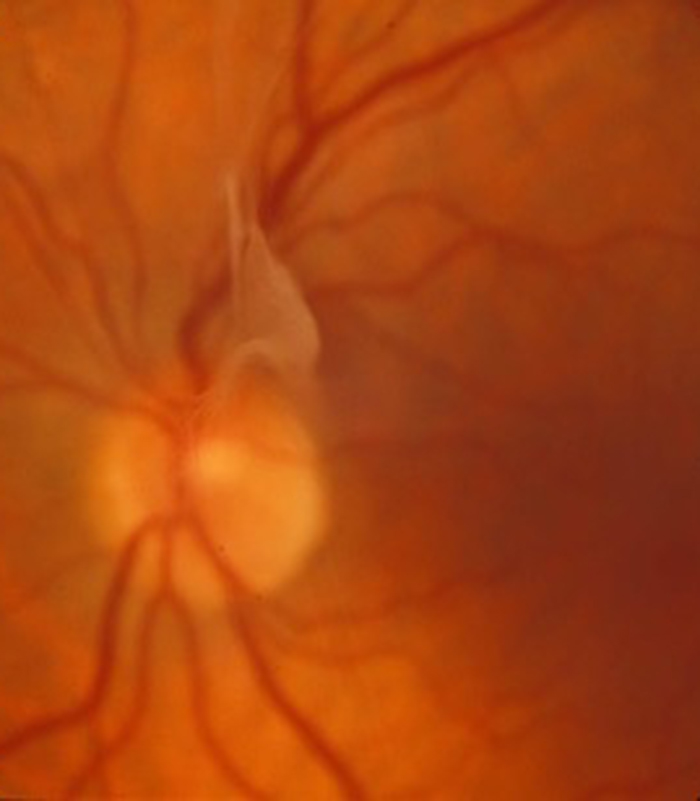
The retina (photographic film at the back of the eye) has a single large vein called the central retinal vein and if this is blocked results in a condition called a central retinal vein occlusion (CRVO) which affects the whole circulation of the retina with general blurring of vision in one eye. Sometimes one of the smaller veins blocks instead and this is called a branch retinal vein occlusion (BRVO). This will affect a patch of the retina and cause a patch of blurred vision in one eye. Most patients with retinal vein occlusions have high blood pressure as an underlying cause and so blood pressure control is very important.
It is rare that both eyes are affected at the same time with this condition.
The poor circulation in the retina results in two problems, blockage of blood vessels and leakage from blood vessels. If leakage occurs in the central part of the retina (macula) it results in the retina becoming thickened and waterlogged (oedema) and therefore not able to function well and you become aware of blurring of vision.
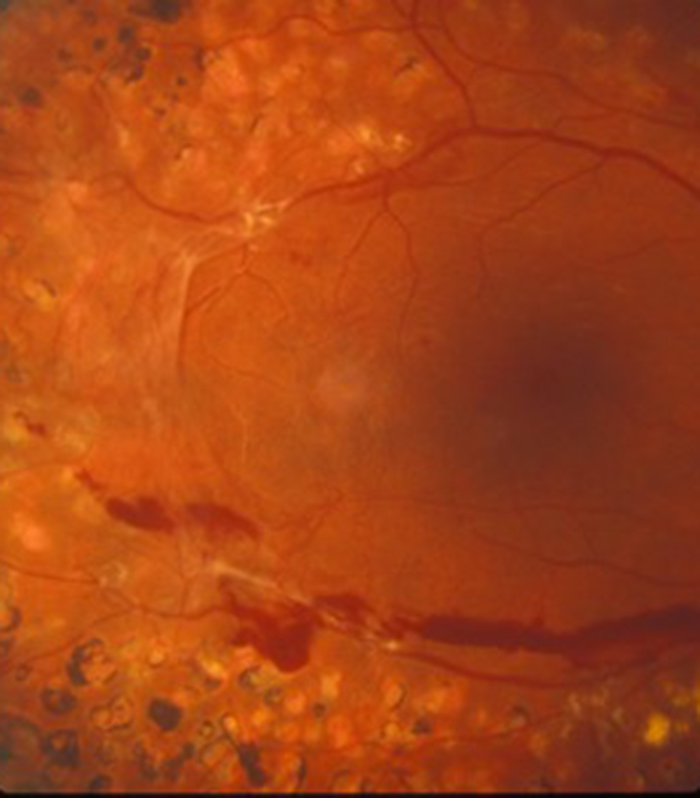
If blockage is the main problem then the body tries to improve the circulation by producing new blood vessels. Some of these blood vessels are helpful by bypassing the blockage and they are called collateral blood vessels. Unfortunately some of the blood vessels are not helpful as they either grow from the retina into the clear jelly (vitreous) that occupies the main eye cavity (usually seen with BRVO) or grow at the front of the eye on the iris (coloured part of the eye) and this is usually seen in patients with severe CRVO.
The blood vessels that grow into the jelly can rupture resulting in haemorrhage into the jelly and patients often notice sudden large floaters and blurring of vision. When blood vessels grow on the iris it impairs a circulation of clear fluid called aqueous. The eye has its own pressure (above atmospheric pressure) that is required in order for it to function and this eye pressure is a result of a balance between the production of aqueous by the eye and drainage of aqueous from the eye.
This eye pressure is not the same as blood pressure. The abnormal blood vessel on the iris seen in some patients with severe CRVO are associated with scarring which obstructs the drainage of aqueous from the eye and results in the pressure in the eye increasing. Glaucoma is a condition where the pressure in the eye is too high and these blood vessels on the iris produce a rare but serious type of glaucoma called thrombotic or rubeotic glaucoma. The pressure can become very high with this type of glaucoma resulting in pain and worsening of vision.
What is the treatment of retinal vein occlusion?
Retinal vein occlusions can be associated with high blood pressure so it is important that your blood pressure is checked and treated if needed. It is also worth having a blood test to make sure your blood sugar and cholesterol are not too high and a blood test called a “full blood count” and “plasma viscosity”. This will check that the blood is not “too thick” or “too thin”. Many vein occlusions result in leakage from the small blood vessels called capillaries with water logging and thickening of the retina. This often occurs in the centre of the retina and is called macular oedema and results in blurring of vision. There are several treatments available for this condition. If the macular oedema is mild and is due to a branch retinal vein occlusion (where just a part of the retina is affected by the blockage) then sometimes things can improve spontaneously especially if blood pressure is well treated and brought under control.
Laser treatment has been available for many years for leakage from branch retinal vein occlusion and although used rarely these days, does still have a place in certain types of leakage. It involves giving some drops to numb the surface of the eye and enlarge the pupil then a contact lens is gently placed on the eye to focus the laser beam. You are often aware of a small bright light during the procedure which is the laser aiming beam. The treatment usually lasts a few minutes only and no special precautions need be taken after the treatment. The laser energy used for this technique is kept to a minimum and it is not a painful treatment. Several laser burns are applied in the area of leakage (where the retina is thickened and waterlogged) to try and dry out the area. The treatment is only indicated if the source of leakage is away from the central part of the macula (called the fovea).
The exact reason why this technique reduces the leakage is still not fully understood but if an improvement occurs it takes a few weeks to months to fully have its effect. Laser treatment is still however “destructive” as each laser burn destroys a small area of the retina in the hope of improving the overall situation in the rest of the centre of the retina. Laser cannot be given if there is a large amount of bruising (haemorrhage) at the macula. It is also not possible to perform laser if (as is often the case) the area of leakage affects the central macula (fovea) as laser to this area (because it is a destructive process) would result in loss of central vision. Laser treatment for leakage associated with a central retinal vein occlusion (CRVO) has also been shown from studies to not be beneficial for macular leakage associated with a CRVO.
The majority of patients that develop leakage at the macula in association with retinal vein occlusions nowadays have injection treatments. The injections include steroid injections and anti-VEGF drugs.
Steroids are very effective at reducing inflammation. Blockage of the retinal vein as well as causing poor circulation also results in inflammation of the tissues which contributes to the leakage that is seen in retinal vein occlusions. Most people needing steroids to reduce inflammation elsewhere in the body need to take them in tablet form and unfortunately there are a large number of side effects when taking steroids as tablets. Inflammation in the eye however can be treated by a local injection of steroid in or around the eye without all the side effects associated with taking steroid tablets.
Ozurdex (Dexamethasone) is a slow release steroid capsule that is injected into the main eye cavity (vitreous cavity) and slowly dissolves over a period of about 4 months and therefore ensures treatment of inflammation over this period.
The injection is given as a day case procedure in theatre. Drops are given to numb the surface of the eye and then a solution of weak iodine is placed on the surface of the eye and the skin around the eye also cleaned with iodine (unless you are allergic to iodine when another cleaning solution is used). This may sound old fashioned but iodine is still the best thing for quickly destroying any bugs (bacteria) that are on or around the eye and eyelids and therefore minimises the risk of infection. The face is then covered with a light paper drape with a small hole that allows access to the eye that is having the injection. The drape is held away from the face so that you do not feel claustrophobic. A small instrument called a speculum is placed to keep the lids apart and stop you from blinking so sometimes you can be aware of a gentle pressure on the lids that can feel a little strange but is not painful.
You may be asked to look in a particular direction when the local anaesthetic is given. The eye will then be completely numb and you will not feel the injection of steroid. Sometimes you notice a floater soon after the injection but this usually settles as the capsule sinks to the lower part of the eye cavity and out of sight. No stitches are needed. After the injection the drape is removed (sometime there is a little pulling on the skin as it is removed) and an antibiotic drop given.
Sometimes you may be asked to put antibiotic drops into the injected eye four times a day for 5 days to also minimise the risk of infection. This is performed by first washing your hands then gently pulling the lower lid down and away from the eye and placing a drop in the groove created between the inner aspect of the lower lid and the eye. If you think you have “missed” put another drop in as you cannot “overdose” on these eye drops. There are no other “dos or don’t” after the injection.
The ozurdex injection usually starts to dry up the retina within a week or two and, as it does, most patients will also notice an improvement in vision. This effect usually lasts for about 3 to 4 months. The hope is that by this time the circulation is starting to improve on its own but if not the injection can be repeated. There is a 1 in 1,000 to 1 in 2,000 risk of infection with any injection into the eye and this includes the Ozurdex injection. There is also a risk that the pressure in the eye can increase following steroid injections but usually this is a temporary feature and most of the time can be treated by drops alone. Ozurdex however is used with caution if you already have glaucoma and may be contraindicated if you have severe glaucoma. Multiple Ozurdex injections (usually more than 3) will result in cataract formation but this can be successfully treated with surgery.
The anti-VEGF agents Eylea, Lucentis, Vabysmo and Avastin which have been used extensively in wet age-related macular degeneration have also been shown to be effective in treating leakage in both branch and central retinal vein occlusion. The duration of action however is shorter than the Ozurdex injection and does need repeated injections with at least 1 month between injections. The total number of injections needed is variable and depends on the severity and duration of the leakage. A large number of patients with retinal vein occlusion are well treated with the anti-VEGF injections but they may need injections indefinitely to sustain the response. The advantage of Eylea, Lucentis,Vabysmo and Avastin injections is that they can be safely given if the patient is being treated for glaucoma (high eye pressure) as Ozurdex can make glaucoma worse and these injections can be given in a dedicated room as an out-patient procedure with local anaesthetic drops alone.
Problems we can help with
I will explain with the aid of video clips the various eye problems I treat. This includes cataract surgery, refractive lens exchange in patients over 50 and medical and surgical treatments of all retinal and macular problems.
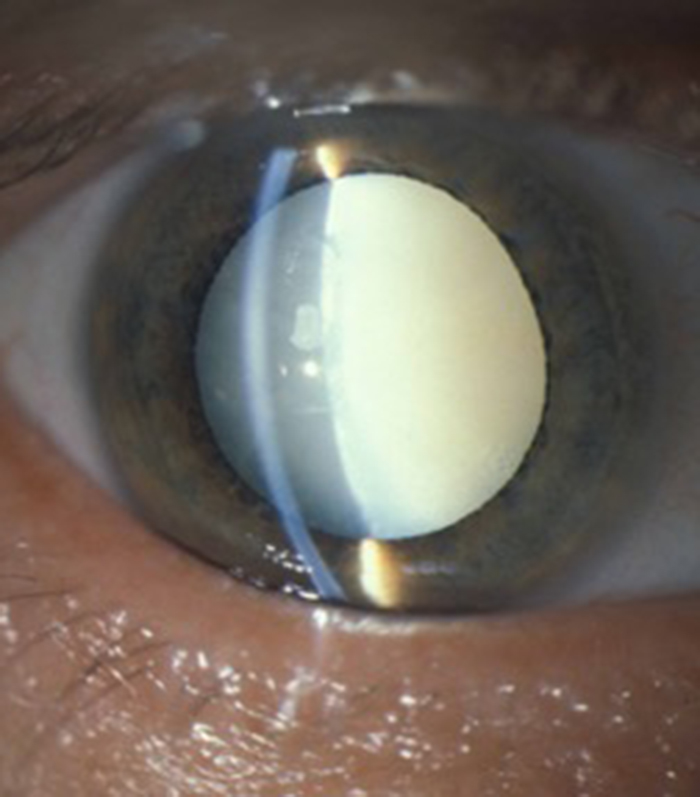
Cataract
I provides advanced micro-incision cataract surgery and will advise on the appropriate intra-ocular lens for your particular needs. This includes toric lenses to correct astigmatism and extended range of vision multifocal lenses to reduce spectacle dependance.
Macular Degeneration
Patients with wet (neovascular) age-related macular degeneration can benefit from prompt injection treatments with various anti-VEGF agents. The first injection can usually be performed on the day of consultation as as "see and treat service".
Retinal Vein Occlusion
Blockage to the veins of the retina can produce significant visual disturbance and may require injection treatments with anti-VEGF agents or steroids at Exeter Eye. More severe cases may require laser or surgery at the West of England Eye Unit under Mr Simcock's care..
Diabetic Eye Disease
Diabetes is becoming increasingly common and can cause significant visual loss. If detected at an early stage vision can be maintained using injection treatments with anti-VEGF agents or steroids. More serious cases may require laser or surgery at the West of England Eye Unit.
Macular Hole
Mr Simcock has pioneered macular hole surgery in the UK and performs a technique which includes lens removal to prevent patients returning for cataract surgery. The technique also benefits from no or limited (2 day) face down posturing to allow hole closure in most macular holes.
Epiretinal Membrane
Scar tissue on the surface of the macular (central retina) causes blurring and distortion of vision. Surgical removal of scar tissue with vitrectomy can be performed if sufficiently troubled. Most patients notice a significant improvement in vision and reduced distortion with this surgery..
Floaters
Patients troubled by floaters in their vision not improving over a period of at least 6 months may benefit from vitrectomy surgery to remove the floaters. Patient selection is important and depends on age (usually over 50) and the state of the jelly (vitreous) in the main eye cavity.

