Are floaters in the vision something to worry about?
The eye is like a camera with the lenses at the front and the photographic film (retina) at the back and between the two in the “body” of the camera is a clear jelly called vitreous. The jelly is not of uniform consistency and usually even young and healthy people have smaller clumps of condensed jelly floating around.
These small floaters are normal and usually are seen when you look at a plain surface such as a white wall or when looking at a clear blue sky. With the passage of time however most of the jelly starts to degenerate and turn to a more watery consistency. Eventually the remaining jelly that is up against the retina or photographic film at the back of the eye suddenly pulls away and collapses down into smaller lumps. This is called a “posterior vitreous detachment or separation”. It usually produces a sudden shower of new floaters and sometimes is associated with transient flashing light sensations. In most people the jelly “lets go” of the retina as it pulls away and does not cause any problems and the floaters usually improve with the passage of time as the brain learns to ignore them or they sink with gravity to the bottom of the main eye cavity (vitreous cavity) and out of the visual axis and so are not noticed.
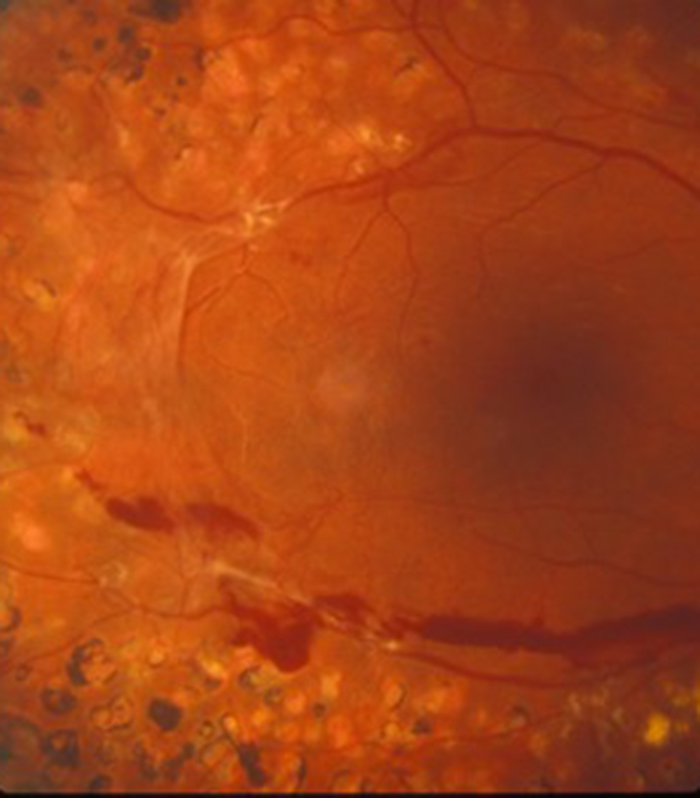
A small number of people are born with abnormal adhesion or stickiness between the jelly and retina in certain places in the peripheral retina. In youth and early middle age it does not cause any problems but once the jelly starts becoming more watery and the remaining jelly wants to pulls away in this region it does not want to “let go” of the retina and pulls on the retina hard enough to tear it away from the back wall of the eye. This usually produces a more pronounced shower of new floaters and is often associated with flashing light sensations. If you push on your eye accidentally with a finger through the eyelid it creates a flashing light sensation which is due to mechanical stimulation to the retina with the pushing force of the finger. The flashing lights produced as the jelly pulls on the retina is created in a similar way but this time it is pulling from the inside rather than pushing from the outside.
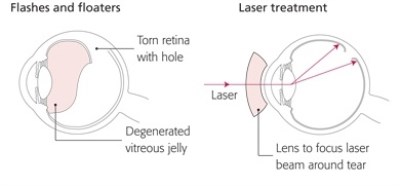
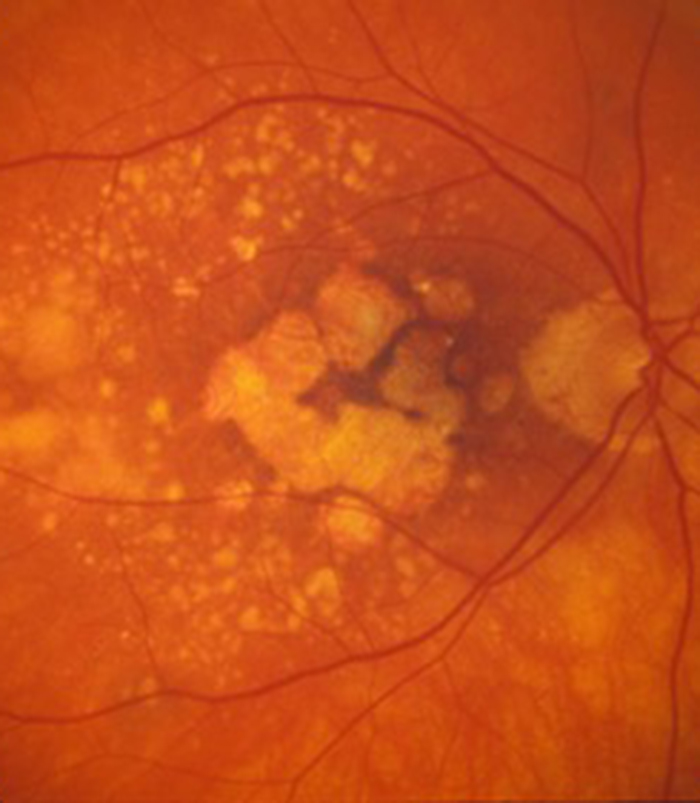
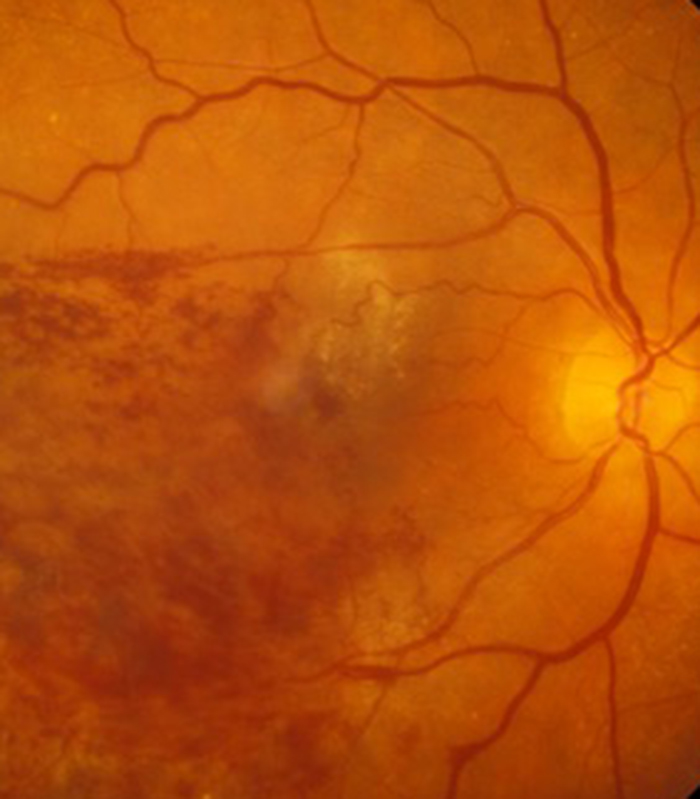
Anyone with sudden onset of flashing lights associated with a new shower of floaters must be assumed to have a retinal tear until proved otherwise and needs to be seen by an eye doctor with a degree of urgency. A tear in the retina is easily treated with laser as an out-patient procedure to “spot weld” it in place and prevent retinal detachment formation. If left untreated however the watery component of the jelly will pass through the tear and under the retina causing it to detach from the back wall of the eye. When this occurs it comes away from one of its blood supplies and a dark shadow appears in your peripheral vision which corresponds to the area of the detachment. This will then progress over hours or days and the dark shadow that you cannot see though will move towards the centre of your vision and then eventually there will be no vision at all in the eye if left untreated. It is therefore very important to see and treat a retinal tear as an out-patient procedure to avoid a formal surgical procedure to reattach the retina which requires a gas bubble to be placed into the eye cavity and for you to posture for a variable period of time after the surgery. If you are unlucky enough to develop a detachment it is better if this can be treated early on in its development (with the shadow still in the peripheral vision) before the central retina (macula) and therefore central vision is affected as once the macula detaches it may not function quite as well even if it is reattached surgically compared to it not detaching in the first place.
A small number of patients are very troubled by their floaters. Patients who are short sighted (myopic) can in particular have difficulty with excessive floaters but they can affect all types of patient. If you develop a sudden appearance of significant floaters you first need to have an urgent eye check to exclude a retinal tear. If no tear is seen but the floaters are very troublesome I would suggest waiting at least 6 months to see if the symptoms improve (the floaters can “float” to the bottom of the main eye cavity with gravity and out of your vision or the brain learns to ignore them).
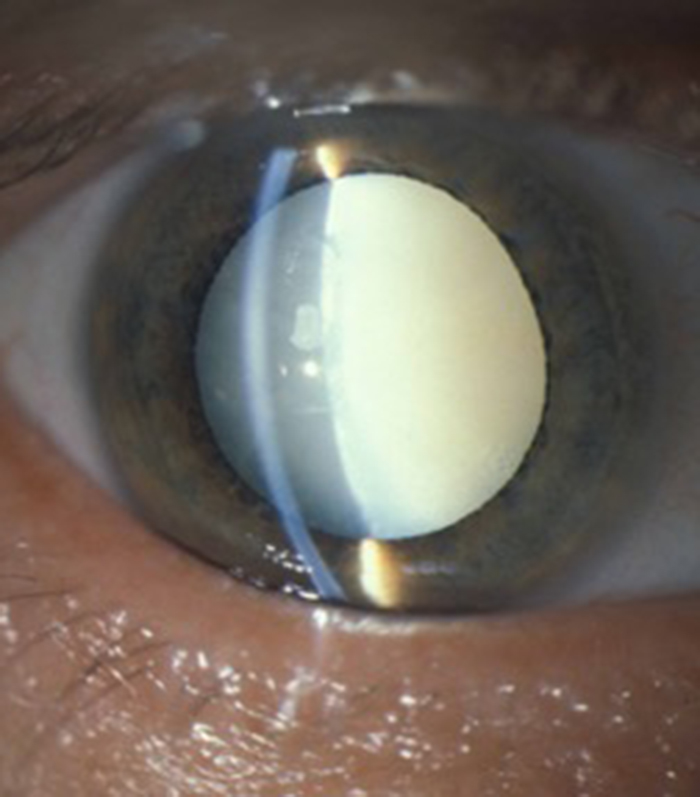
If after 6 months you are still troubled then surgery may be indicated. Laser treatment for floaters is relatively ineffective and treatment is by removing the jelly that contains the floaters that occupies the main eye cavity. This operation is called a vitrectomy and is usually very successful in treating the floaters but patient selection as always is paramount. If you are still of an age where you are able to focus for distance and near without the need for glasses (usually under the age of 45 to 50) then I would be very cautious about recommending surgery. The vitrectomy operation usually results in cataract formation requiring further surgery at a later date (although sometimes the lens can be removed at the same time as the vitrectomy operation, a procedure called “combined surgery”). If you are a younger patient you may find that you need to wear reading glasses sooner than you expected. The success of surgery also depends on the state of the vitreous. If the vitreous has already liquified and you have a vitreous separation then the operations is technically much simpler and with lower risk. If you have floaters but the vitreous is still in the jelly like state and not liquified then surgery is technically more demanding with a greater risk of retinal tear formation at the time of vitrectomy surgery and you will then need additional laser at the time of the operation and also a gas bubble placed in the eye and the need to posture for a period of time following surgery. Vitrectomy surgery for floaters is usually done under local anaesthetic with sedation but can be done asleep (general anaesthetic) if you are particularly anxious. Both are performed as a day-case procedure with no need to stay in hospital overnight.