What is dry eye?
The eye is like a camera with the lens at the front and the photographic film or retina at the back of the eye. The main focusing lens is called the cornea which is the clear window at the front of the eye (where the contact lens is placed if you are a contact lens wearer).
The front surface of the cornea is exposed to the air in the atmosphere and needs to remain smooth, clear and shiny if it is to function properly as a powerful lens that focuses light accurately to the back of the eye. The cornea is covered by a fluid layer called tears and the surface of the cornea is being continually wiped with tears (when awake) by the blinking of the lids.
The film of tears on the surface of the eye is in fact made up of 3 important layers. The first layer is a layer of mucous produced by special cells called goblet cells from the conjunctiva which is the skin that covers the white of the eye. This acts as a “wetting agent” to allow the next layer to stick to it. The second layer is the main watery layer of the tear film and is produced by the lacrimal glands that are situated behind the outer aspect of the upper lids. These glands are very similar to the salivary glands that produce saliva in the mouth and some conditions that produce dry eye can also produce a dry mouth. The third and final layer is a thin oily layer which floats on the surface of the watery layer (oil floats on water) and prevents the water from evaporating and so traps the water and keeps the water there for longer. This fine high quality oil is produced by a series of glands in the lids called meibomian glands and the gland opening or pores are all along the lid margin just behind where the lashes come out.
Dry eye can be due to a deficiency in all, some or just one of these layers and results in the eyes feeling gritty and sore and can also cause transient blurring of vision that improves with blinking. In most cases of dry eye there is no underlying health problem but some patients with rheumatoid disease can have dry eye and also a dry mouth mainly due to a problem with the watery component due to poor function of the lacrimal (and salivary) glands. Patients with blepharitis (a sterile inflammatory change on the lid margins) can also suffer from dry eye as the oil layer may be deficient due to the meibomian glands producing oil that is too thick and blocks the pores of the glands as well as not providing a good oil layer to the tears and therefore allowing the water to evaporate quickly and the eye to dry.
What is the treatment for dry eye?
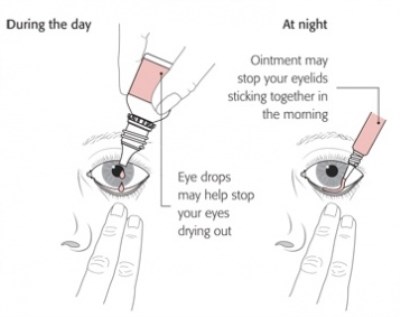
Treatment of dry eye is mainly replacing the poor tears with artificial tear drops. There are numerous artificial tear drops on the market and to a certain extent it is a question of trial and error. There has however been a great deal of research into this area with many new types of artificial tear available in the last few years. The most important advance has been the development of preservative free drops that can be kept in a large bottle. Preservative free drops are the best ones to obtain from the chemist. The drops can be instilled into the eyes as much as is needed to keep the eyes comfortable. The length of time drops remain effective depends on the type of drop but some artificial tear drops can be put in every hour during the day to start off if you have severe symptoms and then reduce the frequency of drops as the symptoms improve. If you are putting in other drops such as glaucoma drops make sure you leave at least 5 minutes between drops so that the artificial tear drop does not dilute the effect of the glaucoma drop.
It is also very important if you have blepharitis to treat this with lid hygiene on a regular (at least every morning) basis so that the oily component of the tear film is as healthy as possible.
If the eyes feel very stuck together and sore first thing in the morning on waking it would be advisable to put in a lubricating ointment (such as VitaPOS, lacrilube or simple eye ointment) before you go to bed at night to prevent the eyes drying out when you are asleep. Do not forget however to put the ointment in just before going to sleep as the ointment blurs the vision for a while and would make it difficult to read in bed.
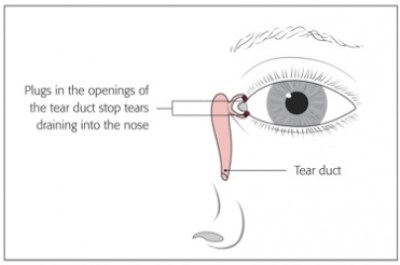
In severe cases of dry eye special plugs called punctal plugs are inserted as an outpatient procedure with anaesthetic drops to block the beginning of the tear passage from the inner aspect of the lids to the nose. Any tears produced (or drops instilled) will therefore stay on the surface of the eye for longer as they will not be able to drain away.
In some patients there is a specific problem with the mucous layer of the tear film resulting in a condition called filimentary keratits where mucous “threads” develop on the cornea and cause discomfort. A specific drop called Ilube (acetylcystine) is used as this drug acts to break up thick mucus.
Very severe cases of dry eye can have a drop called Cyclosporin prescribed. This works over a period of weeks or months and acts in a different fashion to other lubricating drops as this drop helps increase the production of tears from the lacrimal gland rather than just replacing tears. This drop can sting when first instilled and a degree of patience is needed to see if it works as its effect is not immediate.
Problems we can help with
I will explain with the aid of video clips the various eye problems I treat. This includes cataract surgery, refractive lens exchange in patients over 50 and medical and surgical treatments of all retinal and macular problems.
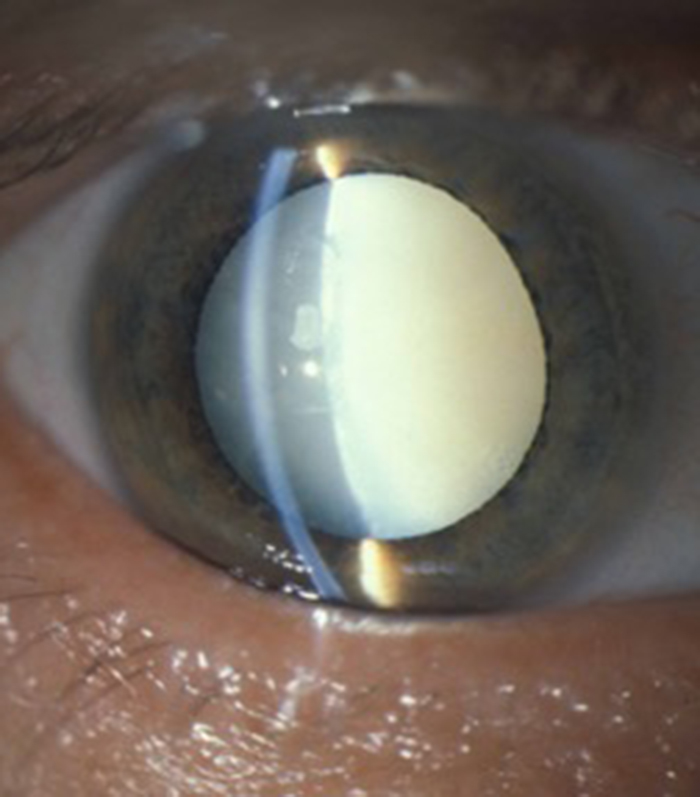
Cataract
I provides advanced micro-incision cataract surgery and will advise on the appropriate intra-ocular lens for your particular needs. This includes toric lenses to correct astigmatism and extended range of vision multifocal lenses to reduce spectacle dependance.
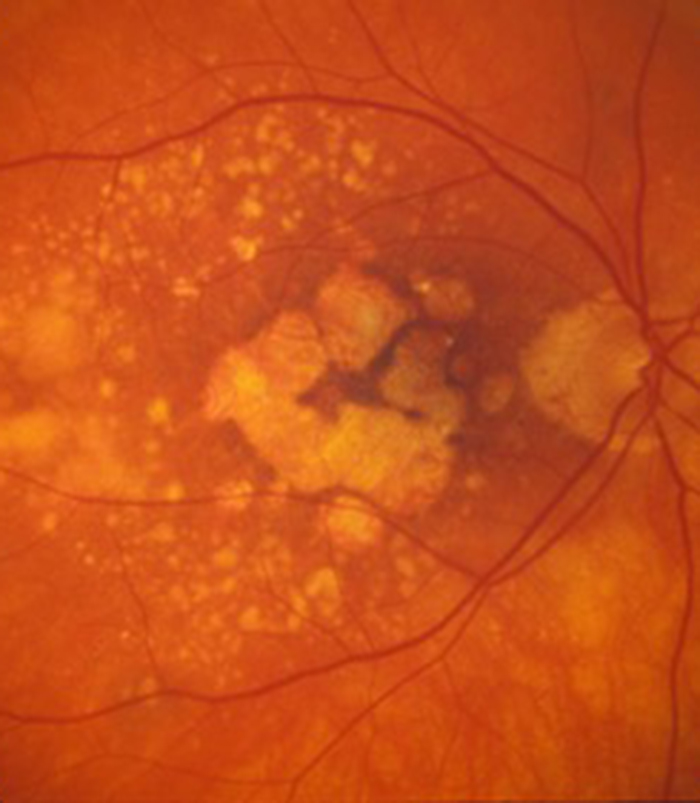
Macular Degeneration
Patients with wet (neovascular) age-related macular degeneration can benefit from prompt injection treatments with various anti-VEGF agents. The first injection can usually be performed on the day of consultation as as "see and treat service".
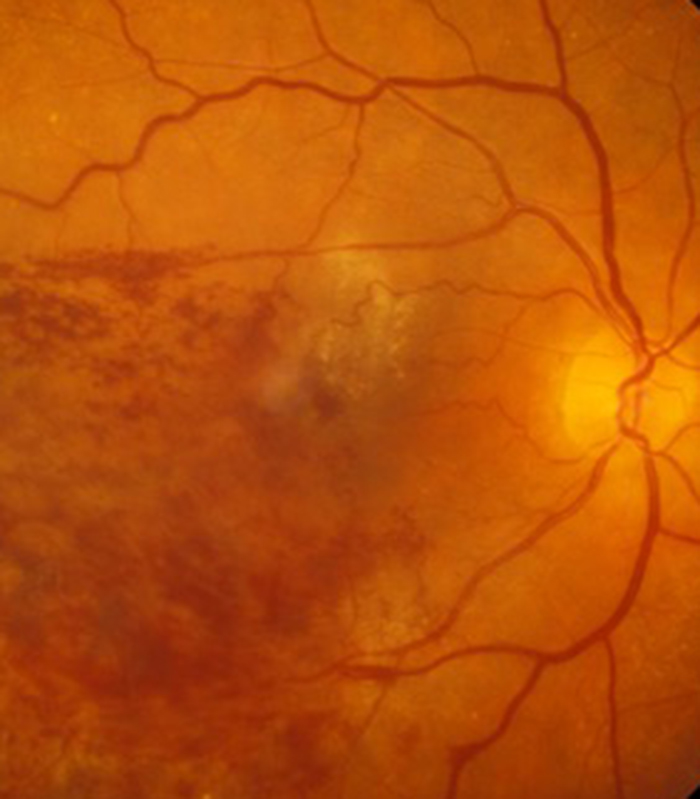
Retinal Vein Occlusion
Blockage to the veins of the retina can produce significant visual disturbance and may require injection treatments with anti-VEGF agents or steroids at Exeter Eye. More severe cases may require laser or surgery at the West of England Eye Unit under Mr Simcock's care..
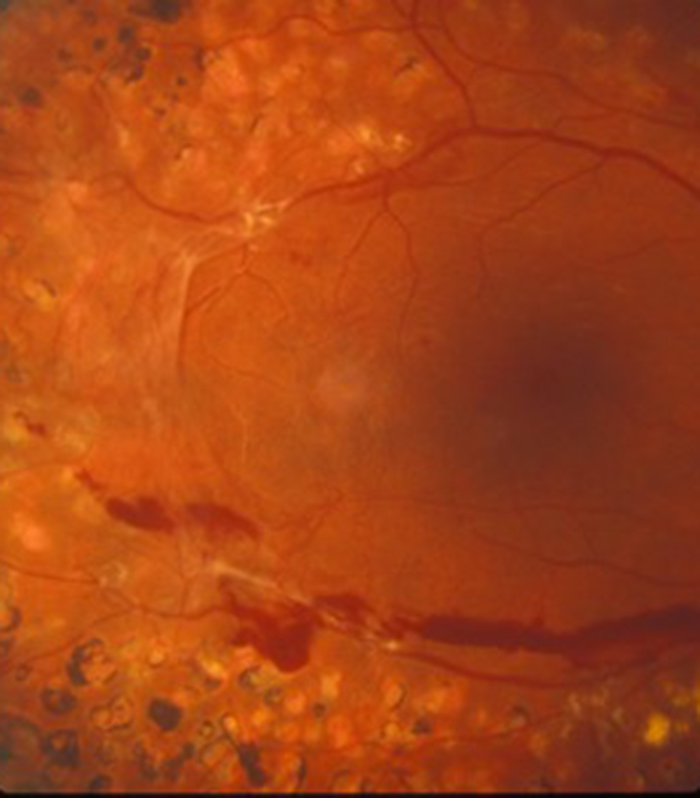
Diabetic Eye Disease
Diabetes is becoming increasingly common and can cause significant visual loss. If detected at an early stage vision can be maintained using injection treatments with anti-VEGF agents or steroids. More serious cases may require laser or surgery at the West of England Eye Unit.
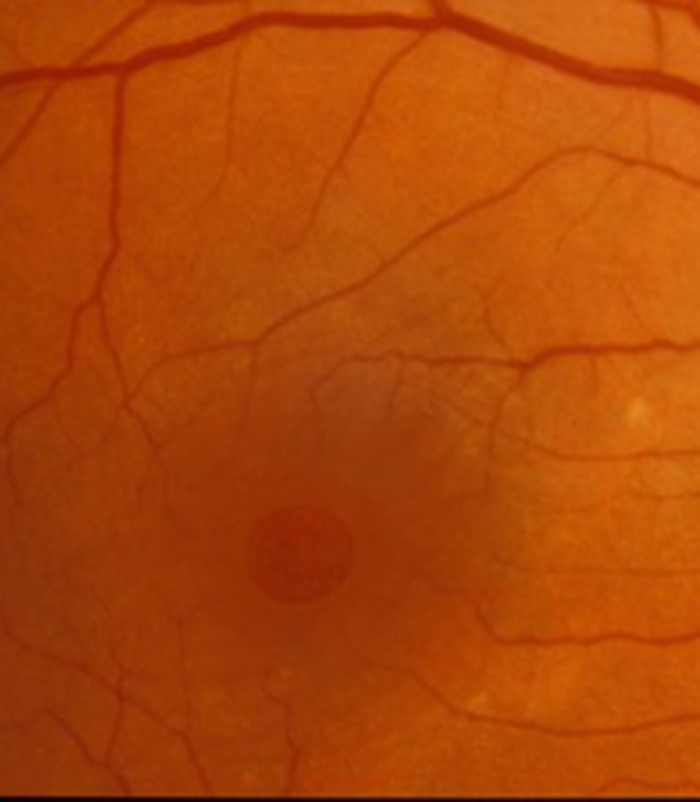
Macular Hole
Mr Simcock has pioneered macular hole surgery in the UK and performs a technique which includes lens removal to prevent patients returning for cataract surgery. The technique also benefits from no or limited (2 day) face down posturing to allow hole closure in most macular holes.
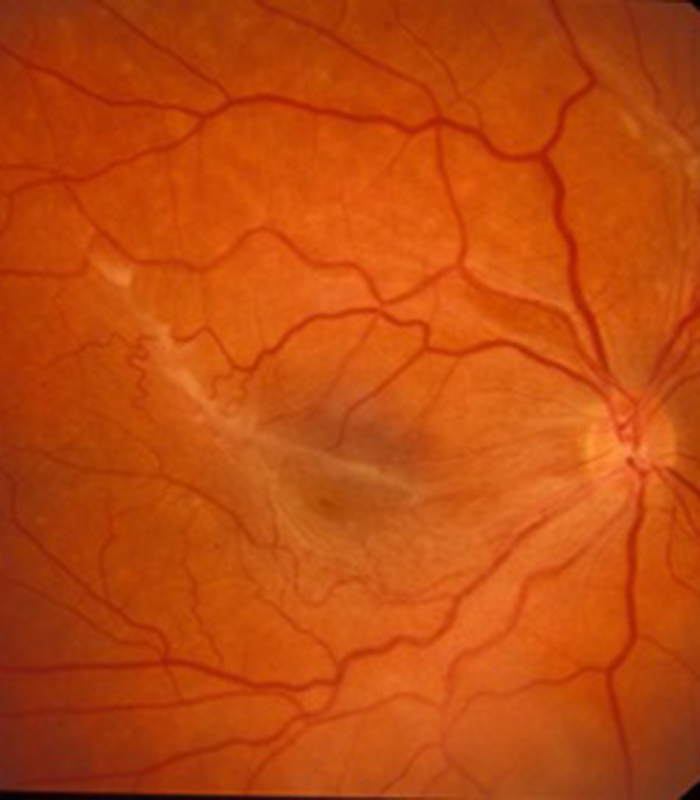
Epiretinal Membrane
Scar tissue on the surface of the macular (central retina) causes blurring and distortion of vision. Surgical removal of scar tissue with vitrectomy can be performed if sufficiently troubled. Most patients notice a significant improvement in vision and reduced distortion with this surgery..
Floaters
Patients troubled by floaters in their vision not improving over a period of at least 6 months may benefit from vitrectomy surgery to remove the floaters. Patient selection is important and depends on age (usually over 50) and the state of the jelly (vitreous) in the main eye cavity.

