What is diabetic eye disease?
Patients are more likely to develop diabetic eye disease the longer they have diabetes and if their diabetic control and blood pressure control are poor. Diabetic eye disease affects the small blood vessels (capillaries) of the retina (photographic film at the back of the eye). The capillaries are where oxygen and sugar are provided to the cells to allow them to function and where the waste products such as carbon dioxide are given back to the blood.
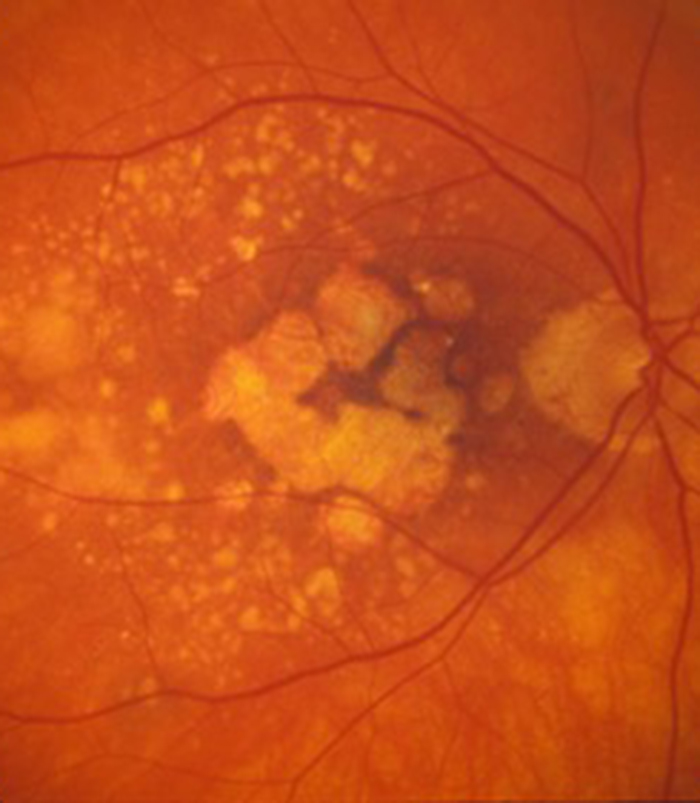
All diabetic eye disease relates to 2 problems with the circulation of the capillaries. The blood vessels can either become leaky or become blocked. The leakage problem is usually seen in older diabetics (although it can happen at any age) and it affects the central part of the retina (macula) and can result in gradual blurring of central vision. The leaky blood vessels result in the macula becoming thickened and waterlogged (often referred to as macula oedema) and also the large fat and protein molecules leak out of the blood vessels and become trapped in the retina (often referred to as hard exudates).
Blockage of blood vessels usually affects the peripheral part of the retina rather than the macula. We mainly rely on central vision from the macula to give us detailed vision for reading, writing, recognising faces and perceiving colour so changes in the peripheral retina (such as blockage of blood vessels) can initially go unnoticed. The retina however tries to improve the circulation by producing new blood vessels but unfortunately they are not helpful as these new blood vessels grow from the retina into the clear jelly (vitreous) that occupies the main eye cavity.
The blood vessels that grow into the jelly can suddenly rupture due to the jelly pulling on them resulting in haemorrhage into the jelly. Patients will then notice sudden large floaters and blurring of vision. If the patient’s central retina (macula) is healthy they would not be aware of these abnormal blood vessels being present until they rupture and cause sudden loss of vision. This is one of the reasons it is so important for diabetic patients to have an annual retinal screening test to look for early signs of both leakage and blockage to the retinal circulation.
What is the treatment of diabetic eye disease?
Diabetic eye disease can be present but go unnoticed and early treatment before visual loss occurs gives you the best chance of maintaining a good level of vision. This is why it is so important to have a screening check of the retina (photographic film at the back of the eye) every year even if you are not noticing any problems. It is also important that both your blood sugar levels and your blood pressure are as well controlled as possible as this gives you the best chance of maintaining a good level of vision.
Diabetic eye disease affects the small blood vessels of the retina called capillaries where the blood gives up its glucose and oxygen to the retinal cells to allow them to function and takes away waste products such as carbon dioxide from the cells. All diabetic eye disease results from two things that can happen to the capillaries. The first is that the capillaries start to leak and the surrounding retina becomes thickened or water logged and this is called macular oedema when it affects the central retina or macula. The second thing that can happen to the capillaries is that they can block resulting in poor circulation to that part of the retina.
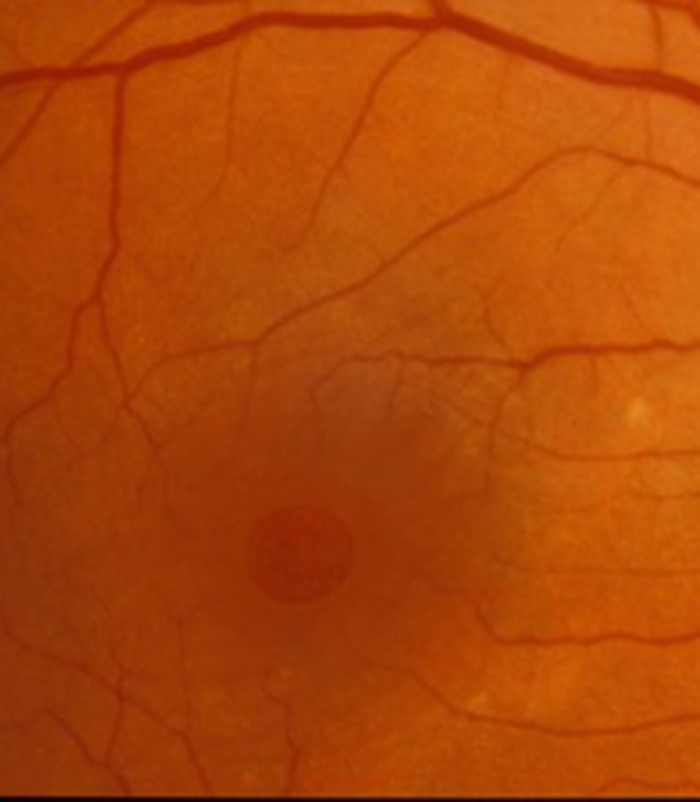
Leakage affecting the central retina (macular oedema) results in a gradual blurring of vision as the retina needs to remain “dry” in order for it to function properly. Leakage tends to occur in patients who develop diabetes when they get older and do not require insulin but can also be seen in younger diabetics on insulin. The leaky capillary has weak walls and usually enlarges and can be seen on retinal photographs taken by the optometrist (optician) as a small red dot called a microaneurysm.
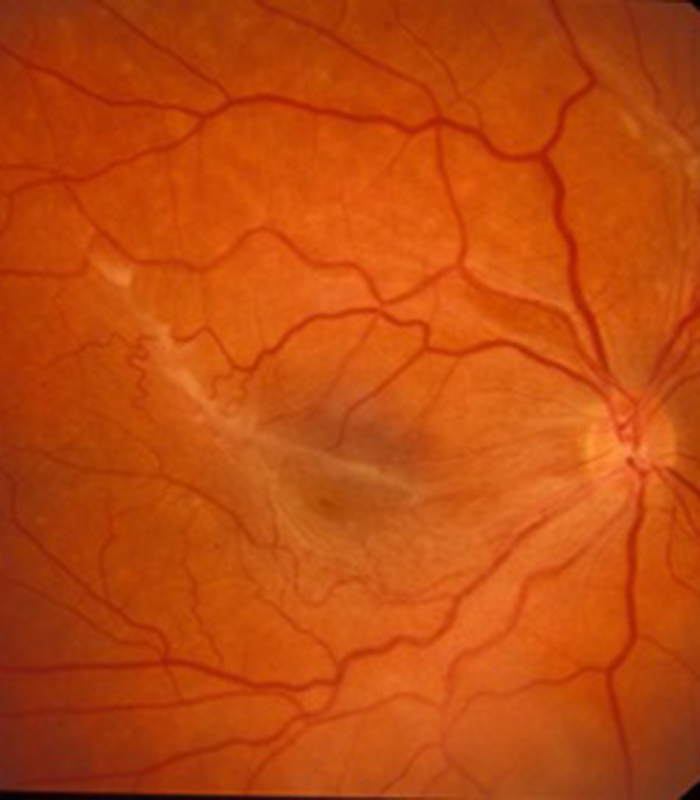
The leakage includes a watery component (oedema) which can get reabsorbed back into the bloodstream but also leakage of large molecules from the blood including blood fat (cholesterol) and blood protein. As these molecules are large it can be difficult for them to get reabsorbed (unlike the watery component) so they get deposited in the retina usually in a ring shape around the leaky microaneurysms and are called hard exudates. The leakage from the microaneurysms can affect a large part of the macula and this is called diffuse leakage or it can affect a small area of the macula (from a smaller number of microaneurysms) when it is called focal leakage. The very centre of the macula is called the fovea and gives the best quality vision and if leakage affects this area it causes the greatest blurring of vision and is called “centre involved” macular oedema. Centre involved macular oedema can be seen with both focal and diffuse oedema.
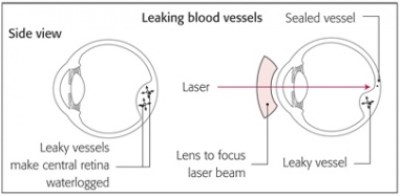 A treatment for macular oedema from leaking microaneurysms in diabetes has been established for many years with laser to the retina but the exact mechanism of action is still not fully understood. A particular type of laser called a green wavelength laser is used to create a small burn on the retina. In patients with focal oedema a small number of laser burns are applied to the centre of the leaky area where the microaneurysms are found. It is thought that by burning the microaneurysm with the laser it causes the blood vessel to “seal” and stop leaking but the exact mechanism is still uncertain. If diffuse oedema is present over a large area of the macula then a grid pattern of laser burns is applied over the area of retinal thickening.
A treatment for macular oedema from leaking microaneurysms in diabetes has been established for many years with laser to the retina but the exact mechanism of action is still not fully understood. A particular type of laser called a green wavelength laser is used to create a small burn on the retina. In patients with focal oedema a small number of laser burns are applied to the centre of the leaky area where the microaneurysms are found. It is thought that by burning the microaneurysm with the laser it causes the blood vessel to “seal” and stop leaking but the exact mechanism is still uncertain. If diffuse oedema is present over a large area of the macula then a grid pattern of laser burns is applied over the area of retinal thickening.
Any centre involved macular oedema (at the fovea) cannot be directly treated with laser as a burn in the very centre of the retina will result in a scar which will cause immediate and permanent loss of central vision. Centre involved macular oedema is now treated with the anti-VEGF drugs Eylea, Lucentis, Vabysmo and Avastin which are injected into the eye. Laser treatment for diabetic leakage still has a place in certain situations and in particular focal leakage that is well away from the centre of the macula (fovea). Most patients however have leakage close to or at the centre of the macula and the current gold standard of treatment is with the anti-VEGF injections. They are given with anaesthetic drops alone in a dedicated eye room as an out-patient procedure and do not require a formal theatre environment. A course of 3 to 5 injections is given in the affected eye (or both eyes if both have problems) once a month over 3 to 5 months and then an assessment is made regarding how effectively it has improved the oedema and hopefully improved the vision. Further injections may be needed and a treatment regimen is tailored and titrated to your particular needs. Sometimes no more injections are needed, sometimes things remain stable for a while then further injections are needed and sometimes continued injections are needed to maintain the response. If after 3 to 5 injections the retina remains waterlogged and vision reduced a decision needs to be made about changing over to a steroid based injection called Ozurdez (see the section on vein occlusions for details of this type of injection). Ozurdex is a slow release steroid pellet and suppresses inflammation as well as also providing an anti-VEGF effect.
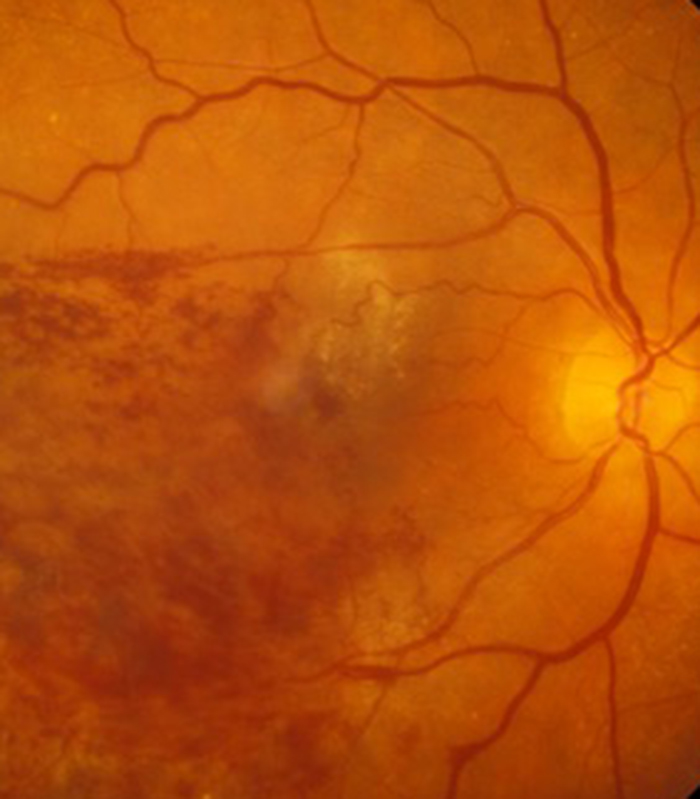
If the problem with the capillaries is one of blockage rather than leakage then a different problem develops in the retina. Leakage as we have seen tends to affect the centre of the retina (macular oedema) and causes gradual blurring of vision. Blockage of capillaries tends to affect the peripheral part of the retina and if the macula is not affected by blockage or leakage then the vision can initially be completely normal and the patient unaware they have problems with poor circulation in their peripheral retina.
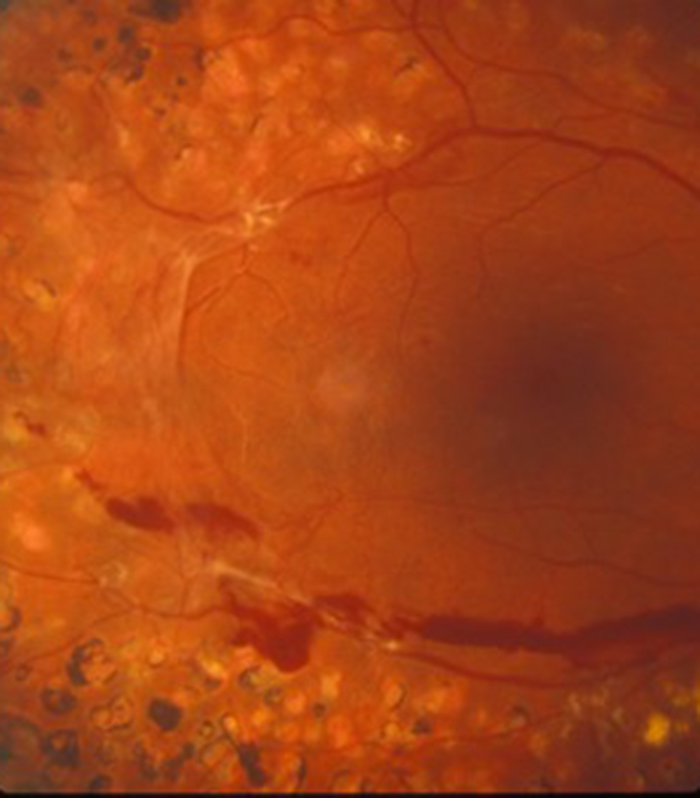
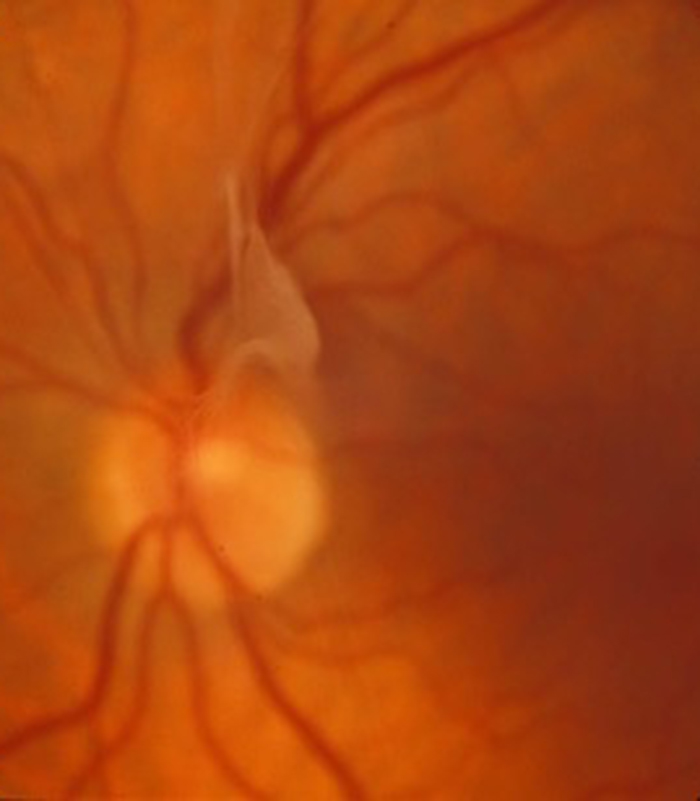
In severe blockage the retina produces new blood vessels which you would think would help the situation. This is called proliferative retinopathy (with everything else being called non-proliferative retinopathy) and unfortunately the new blood vessels grow from the retina into the main eye cavity called the vitreous cavity which is full of a clear jelly called vitreous. Eventually the vitreous pulls on the blood vessels causing them to rupture with a sudden haemorrhage occurring into the vitreous cavity. The patient suddenly notices a large number of floaters and blurring of vision having previously not been aware of any problem with their vision. This is called a vitreous haemorrhage. Treatment for proliferative diabetic retinopathy also includes treatment with the green laser but instead of the burns being applied in small numbers to the macular area (as occurs when leakage is treated) it requires extensive laser to the peripheral retina and this is called pan retinal photocoagulation or PRP. It can only be given when there is still a view of the retina and if a significant vitreous haemorrhage has occurred it is too late and the haemorrhage will either have to settle gradually of its own accord or the haemorrhage will have to be removed surgically (a vitrectomy operation) before the laser can be applied. It is therefore so important to see these abnormal blood vessels before they rupture and again this is the reason why annual retinal screening is so important.
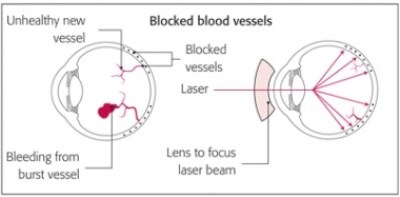 Pan retinal photocoagulation is given as an outpatient procedure with a contact lens applied to the eye (as is focal and grid laser in patients with macular oedema). Drops are placed on the eye to numb the surface of the eye and enlarge the pupil prior to the contact lens being applied. Some patients requiring the more extensive PRP laser may benefit from a local anaesthetic injection as well and if you find the laser is becoming uncomfortable do not hesitate to ask your surgeon to give a local anaesthetic injection as it can usually be given there and then and you would not need to return for a further appointment. A red laser aiming beam is seen during the treatment and the laser does produce a bright flash of light. The full effect of both focal, grid and PRP laser takes several months to take effect and so you need a review appointment between 6 weeks to 3 months following laser treatment. Sometimes PRP laser has to be given over more than one outpatient sessions if extensive laser is required.
Pan retinal photocoagulation is given as an outpatient procedure with a contact lens applied to the eye (as is focal and grid laser in patients with macular oedema). Drops are placed on the eye to numb the surface of the eye and enlarge the pupil prior to the contact lens being applied. Some patients requiring the more extensive PRP laser may benefit from a local anaesthetic injection as well and if you find the laser is becoming uncomfortable do not hesitate to ask your surgeon to give a local anaesthetic injection as it can usually be given there and then and you would not need to return for a further appointment. A red laser aiming beam is seen during the treatment and the laser does produce a bright flash of light. The full effect of both focal, grid and PRP laser takes several months to take effect and so you need a review appointment between 6 weeks to 3 months following laser treatment. Sometimes PRP laser has to be given over more than one outpatient sessions if extensive laser is required.
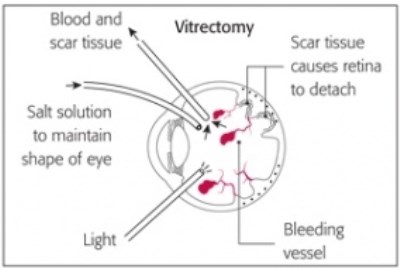 If a vitreous haemorrhage has already occurred it can sometimes spontaneously improve over weeks or months but if the haemorrhage is extensive, recurrent or does not improve quickly it can be removed by an operation called a vitrectomy. This can be performed under local or general anaesthesia usually as a day case procedure. Three very small incisions are created in the sclera (white of the eye) and fine instruments are placed through the incisions to remove the vitreous jelly. As the vitreous is being removed it is replaced by a saline (salt) solution to stop the eye from collapsing and this is gradually replaced after the surgery by a clear fluid called aqueous produced by the eye.
If a vitreous haemorrhage has already occurred it can sometimes spontaneously improve over weeks or months but if the haemorrhage is extensive, recurrent or does not improve quickly it can be removed by an operation called a vitrectomy. This can be performed under local or general anaesthesia usually as a day case procedure. Three very small incisions are created in the sclera (white of the eye) and fine instruments are placed through the incisions to remove the vitreous jelly. As the vitreous is being removed it is replaced by a saline (salt) solution to stop the eye from collapsing and this is gradually replaced after the surgery by a clear fluid called aqueous produced by the eye.
In patients with very severe proliferative diabetic retinopathy the new blood vessels are accompanied by scar tissue which can contract and distort and detach the underlying retina. In this situation more extensive vitrectomy surgery is required to remove the scar tissue. Sometimes the scar tissue may contract and pull open a hole in the retina causing a retinal detachment. This also needs urgent surgery. Patients with severe diabetic proliferative retinopathy with significant scar tissue require technically very demanding surgery and unfortunately the prognosis can be poor in some of these situations. Sometimes a clear oil has to be put inside the eye to stop the retina detaching which requires a further operation to remove some months later once the retina has stabilised. Regular screening should stop patients falling into the category of severe proliferative disease and this is why screening is so important.
Problems we can help with
I will explain with the aid of video clips the various eye problems I treat. This includes cataract surgery, refractive lens exchange in patients over 50 and medical and surgical treatments of all retinal and macular problems.
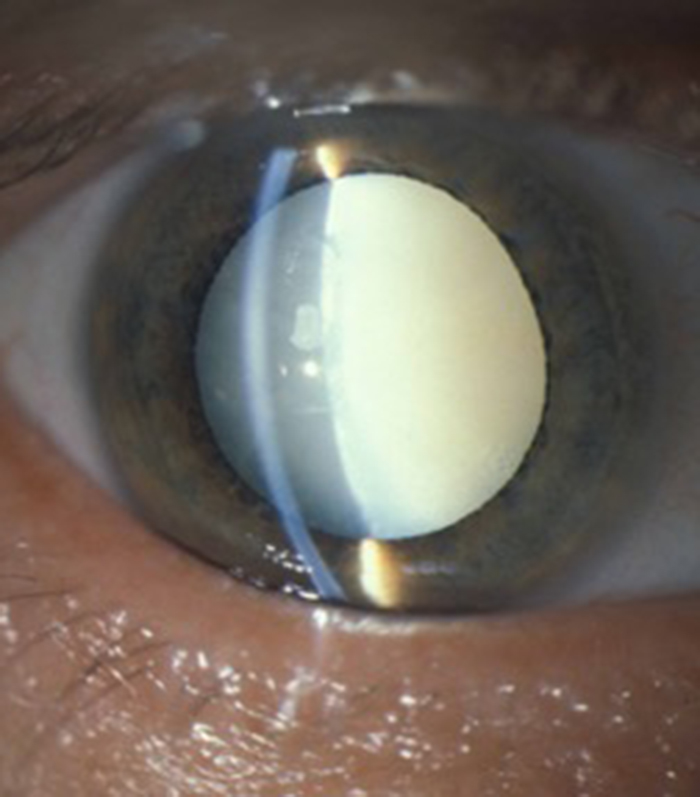
Cataract
I provides advanced micro-incision cataract surgery and will advise on the appropriate intra-ocular lens for your particular needs. This includes toric lenses to correct astigmatism and extended range of vision multifocal lenses to reduce spectacle dependance.
Macular Degeneration
Patients with wet (neovascular) age-related macular degeneration can benefit from prompt injection treatments with various anti-VEGF agents. The first injection can usually be performed on the day of consultation as as "see and treat service".
Retinal Vein Occlusion
Blockage to the veins of the retina can produce significant visual disturbance and may require injection treatments with anti-VEGF agents or steroids at Exeter Eye. More severe cases may require laser or surgery at the West of England Eye Unit under Mr Simcock's care..
Diabetic Eye Disease
Diabetes is becoming increasingly common and can cause significant visual loss. If detected at an early stage vision can be maintained using injection treatments with anti-VEGF agents or steroids. More serious cases may require laser or surgery at the West of England Eye Unit.
Macular Hole
Mr Simcock has pioneered macular hole surgery in the UK and performs a technique which includes lens removal to prevent patients returning for cataract surgery. The technique also benefits from no or limited (2 day) face down posturing to allow hole closure in most macular holes.
Epiretinal Membrane
Scar tissue on the surface of the macular (central retina) causes blurring and distortion of vision. Surgical removal of scar tissue with vitrectomy can be performed if sufficiently troubled. Most patients notice a significant improvement in vision and reduced distortion with this surgery..
Floaters
Patients troubled by floaters in their vision not improving over a period of at least 6 months may benefit from vitrectomy surgery to remove the floaters. Patient selection is important and depends on age (usually over 50) and the state of the jelly (vitreous) in the main eye cavity.

