What is a cataract?
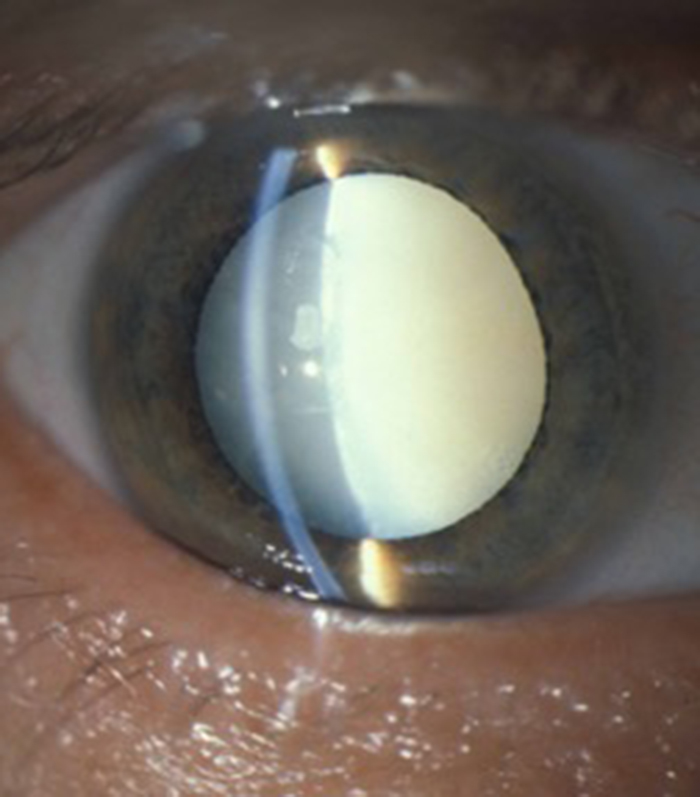
The eye is like a camera with lenses at the front and a photographic film (retina) at the back. There are two lenses in the camera, the cornea (clear window at the front of the eye where contact lenses are placed) which does most of the focusing of the eye (coarse focus) and the lens inside the eye which is the fine focus system of the camera. A cataract is a cloudy lens inside the eye.
The treatment for cataract is to remove the cloudy lens and replace it with a new clear plastic lens called an intra-ocular lens. The timing of a cataract operation is when you the patient are sufficiently troubled to wish to proceed with surgery. If you are happy with your present quality of vision then it is unlikely that surgery would be needed at this moment in time. Cataracts do not improve and usually slowly progress with increased blurring of vision or glare symptoms over months or years. They usually affect both eyes but often affect one eye more than the other.
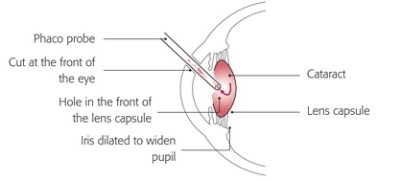
How is cataract surgery performed?
Before the operation a measurement has to be taken of the shape of the eye with a machine called an IOL master. This is a very accurate, totally painless assessment of the eye. It just requires you to look at a red spot of light and measures the curvature of the cornea at the front of the eye and the length of the eye from front to back. Each eye is slightly different in shape but with these two measurements the machine calculates an accurate strength of focus for the new lens implant (called an intra-ocular lens or IOL) for your particular eye.

Cataract surgery is performed through small incisions at the edge of the cornea (clear window at the front of the eye) and the incisions are so small that they seal by themselves and do not require any stitches. The surgery is performed as a day case procedure in hospital (you do not need to stay overnight) and the operation usually takes about 15 to 20 minutes. Although the surgery takes a short period of time it is likely that you’re stay at Admiral House would be a couple of hours as you need some preparation prior to surgery and a cup of tea or coffee after surgery! Most operations are performed with a local anaesthetic (to numb the eye) but if you are anxious about surgery some sedation can be given by the consultant anaesthetist to help you relax. If you are very anxious surgery can also be performed under general anaesthesia (you are asleep) as a day case procedure. If general anaesthesia is needed the surgery has to be performed at the West of England Eye Unit of the Royal Devon and Exeter Hospital as there are no GA facilities at Admiral House.
You do not have to change your clothes before going into theatre. Drops are given to the eye to be operated on to numb the eye and a small pellet is placed on the inner aspect of the lower lid to enlarge the pupil. You will be asked to lie on a comfortable theatre trolley which has been specially designed to accommodate all requirements for positioning and in particular is comfortable for people with arthritis and can be moved to a “propped up” position if you are breathlessness lying flat. The skin around the eye is then cleaned with an iodine solution (provided you are not allergic to iodine) to minimise the risk of infection. The anaesthetist will then give the injection around (not into) the eye to completely numb it. This is all performed in a room next door to theatre called the anaesthetic room.
The trolley is then moved into the main theatre and positioned under the operating microscope. The skin around the eye is cleaned once more with iodine to again keep the risk of any infection to the absolute minimum. This may sound old fashioned but iodine is still the best thing for quickly destroying any bugs (bacteria) that are on or around the eye and therefore minimises the risk of infection. Do not be worried if you feel the light pressure of the gauze swab cleaning the skin around the eye. This is normal and does not mean the local anaesthetic has not worked. The injection will numb the eye (and therefore you will not feel the operation) but it does not usually numb the sense of touch for the skin around the eye.
The face is then covered with a light paper drape with a small hole that allows access to the eye having surgery. A small “tent” is created with the drape so that it is not up against the face and fresh air is gently blown into the “tent”. A small instrument called a speculum is placed to keep the lids apart and stop you from blinking and sometimes you are aware of a gentle pressure on the lids that can feel a little strange at first but is not painful.
The eye having surgery is now out of your control but you can still blink with the other eye. You can keep this eye open if you wish (you will only see the blue colour of the inside of the drape) but most patients prefer to gently close this eye during the operation. The surgery usually takes 15 to 20 minutes and someone can hold your hand during surgery if you wish. Some patients note that everything goes dark during the operation, some note interesting coloured light sensations and some are aware of shapes moving. There are also some buzzing noises during the surgery which again is completely normal and is the special small incision cataract machine called a phacoemulsifier in action.
There is a moderate amount of fluid passing in and around the eye during the operation. Sometimes it can pass around the drape and give you a hair wash! Do not be alarmed as its only a simple salt water solution.
I often like to listen to music during the operation. With the streaming services now available I am happy to take requests prior to surgery to put on the iPhone!
If you wish to cough or move during the operation you can do as I can come out of the eye with my instruments quickly and safely due to the self sealing wounds. I would just need a brief warning prior to your moving by either putting up your hand if no one is holding it or if you have a hand holder, by giving the persons hand a squeeze. You can then cough or sneeze safely before I return to surgery when you are once more comfortable.
When the operation is over the drape is removed (sometimes there is a bit of pulling on the skin as it is removed) and a clear plastic shield placed on the eye with sellotape. The eye is not usually padded and you can blink normally under the shield. The shield can be removed after a couple of hours and is there to prevent you accidentally touching the eye when it is still numb from the anaesthetic. Some patients are unable to blink at all until the anaesthetic wears off. In this situation an eye pad (with the lid closed under the pad) is placed, again for a couple of hours only until the anaesthetic wears off. It is important after this to keep the eye open and blinking and have the post-operative drops given.
It can be a few hours for the local anaesthetic to wear off. Do not be alarmed if the vision is still very blurred during this period. This is normal. You may also experience double vision or seeing “two of everything”. Again this is normal and due to the local anaesthetic affecting the muscles that move the eye preventing the operated eye moving in the same way as the un-operated eye. The double vision will wear off after a few hours but can be quite disconcerting until it disappears.
The drugs that enlarge the pupil prior to cataract surgery are very powerful and the pupil can stay enlarged for up to 48 hours after cataract surgery. This can result in some residual blurring of vision and bright lights can be a little uncomfortable so dark glasses may be needed if going outside for the first couple of days. The vision should however should improve after a couple of days.
Drops need to be placed onto the surface of the eye four times a day for four to six weeks. This is performed by first washing your hands then gently pulling the lower lid down and away from the eye and placing a drop in the groove created between the inner aspect of the lower lid and the eye. If you think you have “missed” put another drop in as you cannot “overdose” on these eye drops. If you are struggling with this technique another option is to lie down on the bed and look up at the ceiling whilst holding the drop bottle above the eye and squeeing the bottle to get the drop to release. The drops are a combination of steroid (to keep the eye comfortable) and antibiotic (to prevent infection).
The small incisions created at the time of surgery take about 6 weeks to heal. The shape of the eye can change during this healing process and this is why you should not go to the optometrist (optician) to have your glasses updated until the drops have finished.
What are the risks of cataract surgery?
Any operation has a risk but the risks of cataract surgery are very low. There is a one in 2,000 risk of infection or haemorrhage and a one in 10,000 risk of severe complications that result in significant loss of vision.
What can I do after cataract surgery?
Many patients feel they should considerably restrict their activity immediately following cataract surgery but this degree of caution relates to the old fashion operation where a larger wound was created requiring many stitches. With modern small incision cataract surgery there is no problem with bending over or going out for gentle exercise (such as walking) within 24 hours of surgery. It is best to avoid swimming for 4 weeks. Some patients who enjoy Yoga may do inversions but this does increase the pressure of blood in the veins of the eye so I would suggest avoiding this for 2 weeks.
What would suggest something is wrong after cataract surgery?
Complications following cataract surgery are very rare but the “red flag” symptoms that require immediate review are severe pain with increasing blurring of vision, bright lights being very uncomfortable for the eye (not just things being much brighter after cataract surgery), and increasing redness of the eye in association with the previous symptoms. A bright red patch on the white of the eye with good vision and no pain is likely to be a simple bruise associated with the local anaesthetic injection called a sub-conjunctival haemorrhage and although may look alarming will gradually fade over a few weeks. It is often seen in the corner of the eye near the nose. If you are in any doubt it is always best to get an urgent medical review of the situation.
Can I do away with my glasses after cataract surgery?
Patients who are long sighted or short sighted can be made normal sighted (seeing clearly in the distance without glasses) at the time of cataract surgery as the lens implant is calculated so that you do away with your glasses for distance and only need reading glasses. Sometimes a weak strength of glasses is still needed to get the distance vision as good as possible for tasks such as driving at night.
What is astigmatism?
Patients who have astigmatism (the cornea or clear window at the front of the eye is more curved in one direction than the other, like a rugby ball) can also have this treated at the time of surgery. Mild amounts of astigmatism can be improved by placing the incisions required for cataract surgery in the area of the cornea that has the greatest curvature. More severe astigmatism can be very effectively treated with toric lens implants to significantly improve distance vision without glasses. My preference is to think about a toric lens when there is over 1 Diopter of corneal astigmatism and would strongly recommend a toric lens if greater than 1.5 Diopters of corneal astigmatism.
Can I do away with my reading glasses after cataract surgery?
Options for doing away with reading glasses completely are available but to date there is no “perfect solution” resulting in excellent vision at all distance without glasses.
The two current options are “monovision” and multifocal intraocular lens implants.
Monovision
If you have cataract in both eyes, one eye can have an implant set for good distance vision and one eye for near vision. The distance eye is usually your “dominant eye” which is the one you would use when looking down a telescope. The “non-dominant” eye is set for near vision.
The near vision eye can have a close focus for easy reading in bed without glasses but this means a large difference in the focus between the two eyes and some people have difficulty getting used to this difference. This option works best in people who have already been happy with this when using contact lenses to produce the same effect.
Blended monovision (sometimes called mini or micro monovision) is a similar process but the “non-dominant” eye is set at an intermediate distance such as when looking at a computer. The advantage is that the difference between the two eyes is not so great and most people are comfortable with this option and can often read without glasses in a good light. The disadvantage is that reading small print or in poor light may still require weak reading glasses and there does remain some imbalance in focus between the two eyes.
Multifocal intraocular lens implants
The multifocal intraocular lens implant is manufactured to produce multiple images that fall on the retina (the photographic film at the back of the eye) from different distances (far and near and sometimes an intermediate distance as well). The brain learns to ignore the image it does not want and concentrates on the image that is clear at the distance required. The optics of these lenses are quite complicated and not without some compromise in overall quality of vision.
Some people notice glare symptoms and haloes or starburst effects which can be troublesome when night driving. Usually these effects reduce as the brain adapts to your new vision over several months but it can sometimes take up to 6 months to resolve. A very small number of patients are still sufficiently troubled after 6 months to require lens removal.
As the light entering the eye is “divided up” into different focuses there is slightly less light available at each focus compared with the normal monofocal lens where all the light entering the eye has a single focus. This slightly reduces the quality of vision at all distances but this is not particularly noticeable in good light but can be more noticeable in poor light situations such as dawn or dust or in a poorly lit restaurant. This is sometimes called loss of “contrast sensitivity”. This effect may be more noticable as you age or if you develop macular degeneration.
If you need very high quality vision for distance and driving at night (such as HGV drivers) then multifocal lenses should be used with caution. If patients need very high quality vision at near (such as model makers) then it is unlikely that a multifocal implant alone will produce this level of near vision and glasses may also be needed for detailed near visual tasks.
Patients who have previously been myopic (short sighted) and therefore used to good near vision without glasses may be a little disappointed with the quality of near vision that these lenses produce and should be used with caution and with a full explanation of the outcomes in these circumstances.
Multifocal intra-ocular lenses also work best when there is minimal astigmatism present and patients with corneal astigmatism should have toric multifocal intra-ocular lenses to obtain the best possible vision.
Toric lenses, multifocal lenses and Toric multifocal lenses are often termed “premium lenses” and are more expensive than monodical lenses.
Multifocal and extended depth of focus intra-ocular lenses
There is a type of multifocal lens called an extended depth of focus lens (EDoF) that provides a degree of multifocality with a slightly reduced risk of glare and haloes. One lens produced by AMO is called the Tecnis Symphony lens. I have used this lens to good effect in a large number of patients and provides very good distance and intermediate vision and good near vision in adequate lighting but still may requires glasses for near visual tasks if the print is small or the lighting poor. Patient satisfaction with theses lenses is very high and many are spectacle independent.
All intraocular lenses are designed to be easily inserted into the eye at the time of cataract surgery with minimal risk but removal of intraocular lenses is more technically challenging and whilst most of the time can be performed successfully there is a greater risk. It is therefore important to be comfortable with a decision to have either monovision or multifocal lenses and whilst these options are very successful for most people there are some who are not suited and as with all operations patient selection is very important. Multifocals work best if both eyes have surgery, all astigmatism is treated and the retina is healthy.
What if I have cataract and previous laser refractive surgery such as LASIK and PRK or previous Radial Keratotomy?
Does being short sighted increase the risk of cataract surgery?
What is Fuch’s endothelial dystrophy and does this increase the risk of cataract surgery?
Does pseudoexfoliation syndrome increase the risk of cataract surgery?
Can a cataract come back after cataract surgery?
Patients often ask if the cataract will come back after surgery. This does not happen but sometimes laser treatment is needed months or years after cataract surgery. When the cataract is removed, the back surface of the cataract called the posterior capsule is left behind. It is needed to support the intra-ocular lens that is inserted at the time of cataract surgery and also separates the front of the eye from the clear jelly called vitreous that occupies the main eye cavity. If this posterior capsule was removed there would be no support for the lens in its correct position and the lens would fall to the back of the eye. Rupture of this capsular at the time of cataract surgery is a complication that often requires the new lens to be placed in a slightly different position to normal.
This posterior capsule is almost always clear at the time of the cataract operation and therefore allows light to pass through it and focus on the retina or photographic film at the back of the eye. The posterior capsule can however gradually become cloudy with the passage of time (sometimes many years after the original cataract operation) and you would notice the vision once again becoming gradually more blurred and sometimes glare symptoms. . The treatment is to make a central hole in the posterior capsule with laser. It is called a YAG laser capsulotomy after the type of laser required to create the hole.
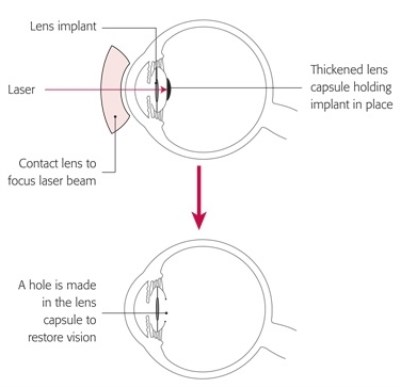 The treatment only takes a few minutes as an outpatient procedure and is therefore a very simple thing to perform. Drops are given to numb the surface of the eye and to enlarge the pupil. A contact lens is then placed on the surface of the eye to allow the laser to focus. You may feel a small amount of gentle pressure on the eye from the contact lens but the posterior capsule has no nerve ending and therefore the laser treatment is completely painless. You may be aware of a red light shining into the eye (which is the aiming beam of the laser) and a clicking sound. The laser treatment only takes a few minutes to complete and creates a hole in the centre of the posterior capsule.
The treatment only takes a few minutes as an outpatient procedure and is therefore a very simple thing to perform. Drops are given to numb the surface of the eye and to enlarge the pupil. A contact lens is then placed on the surface of the eye to allow the laser to focus. You may feel a small amount of gentle pressure on the eye from the contact lens but the posterior capsule has no nerve ending and therefore the laser treatment is completely painless. You may be aware of a red light shining into the eye (which is the aiming beam of the laser) and a clicking sound. The laser treatment only takes a few minutes to complete and creates a hole in the centre of the posterior capsule.
The contact lens is then removed from the eye and you should notice an improvement in vision almost immediately with a further improved over the few hours needs for the effect of the drops that enlarge the pupil to wear off. Sometimes you may be aware of an increase in floaters in the first few days after laser which is due to some of the “debris” from the capsule falling back into the main eye cavity but this quickly improves.
No drops are needed after laser treatment and it does not alter the glasses prescription therefore you do not need to visit your optometrist (optician) after the laser treatment. Once the laser has been performed it lasts forever and does not need to be repeated.
Problems we can help with
I will explain with the aid of video clips the various eye problems I treat. This includes cataract surgery, refractive lens exchange in patients over 50 and medical and surgical treatments of all retinal and macular problems.
Cataract
I provides advanced micro-incision cataract surgery and will advise on the appropriate intra-ocular lens for your particular needs. This includes toric lenses to correct astigmatism and extended range of vision multifocal lenses to reduce spectacle dependance.
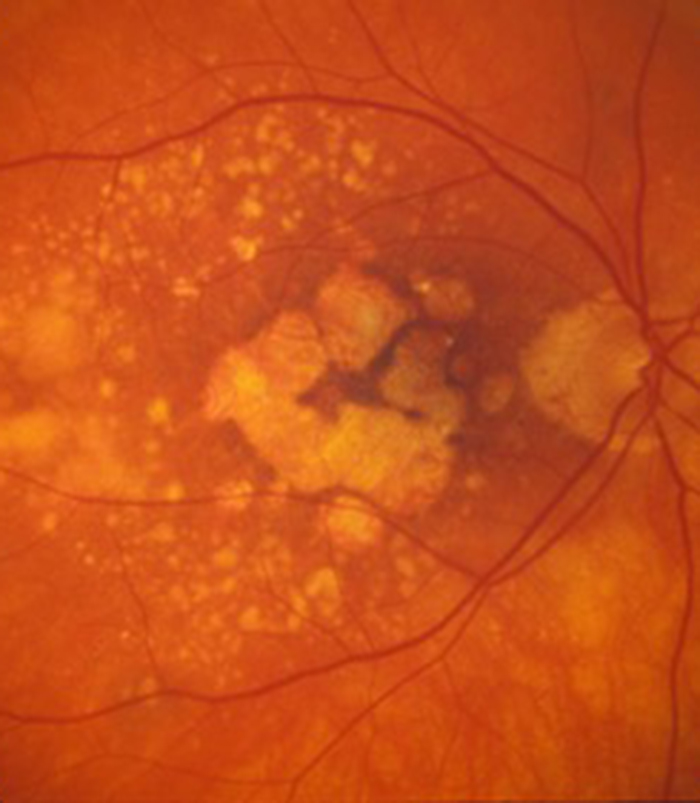
Macular Degeneration
Patients with wet (neovascular) age-related macular degeneration can benefit from prompt injection treatments with various anti-VEGF agents. The first injection can usually be performed on the day of consultation as as "see and treat service".
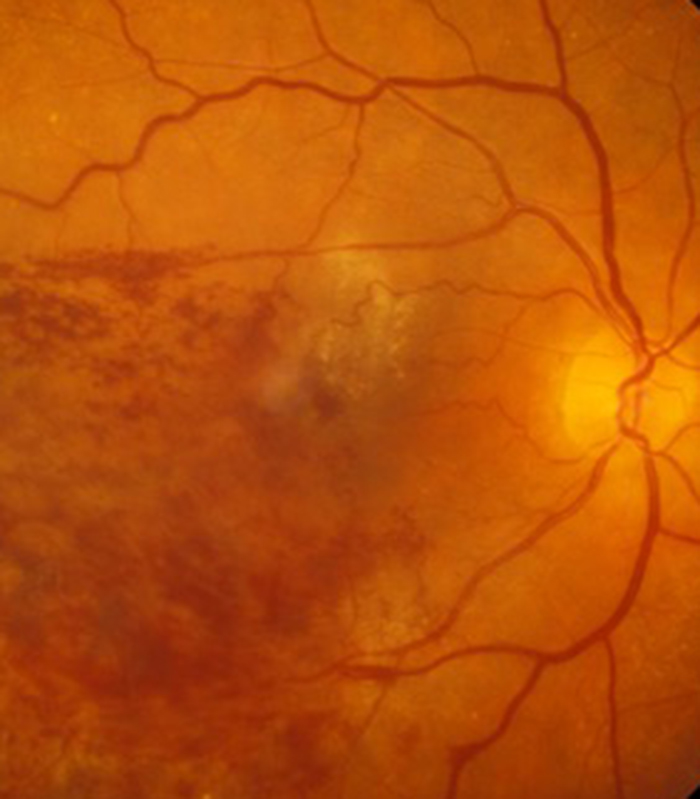
Retinal Vein Occlusion
Blockage to the veins of the retina can produce significant visual disturbance and may require injection treatments with anti-VEGF agents or steroids at Exeter Eye. More severe cases may require laser or surgery at the West of England Eye Unit under Mr Simcock's care..
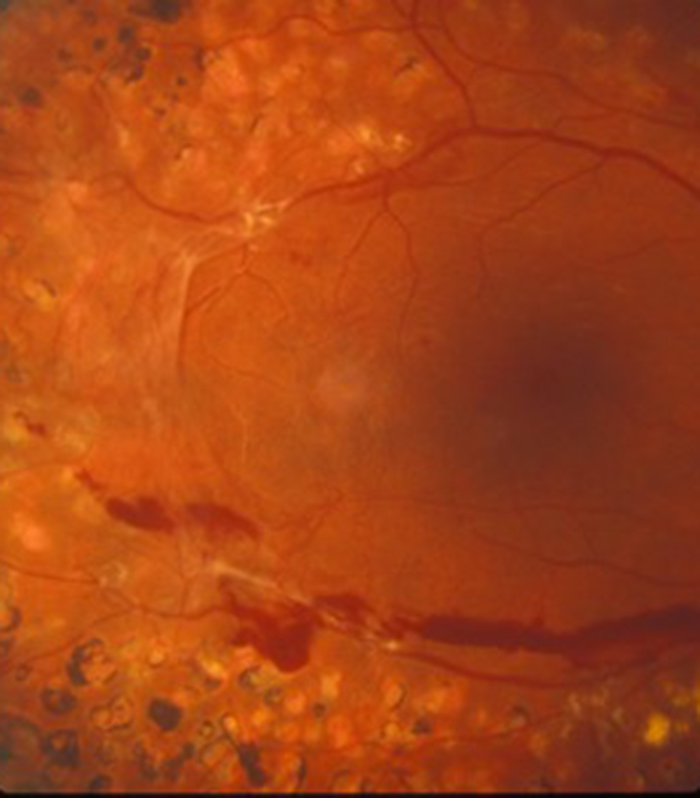
Diabetic Eye Disease
Diabetes is becoming increasingly common and can cause significant visual loss. If detected at an early stage vision can be maintained using injection treatments with anti-VEGF agents or steroids. More serious cases may require laser or surgery at the West of England Eye Unit.
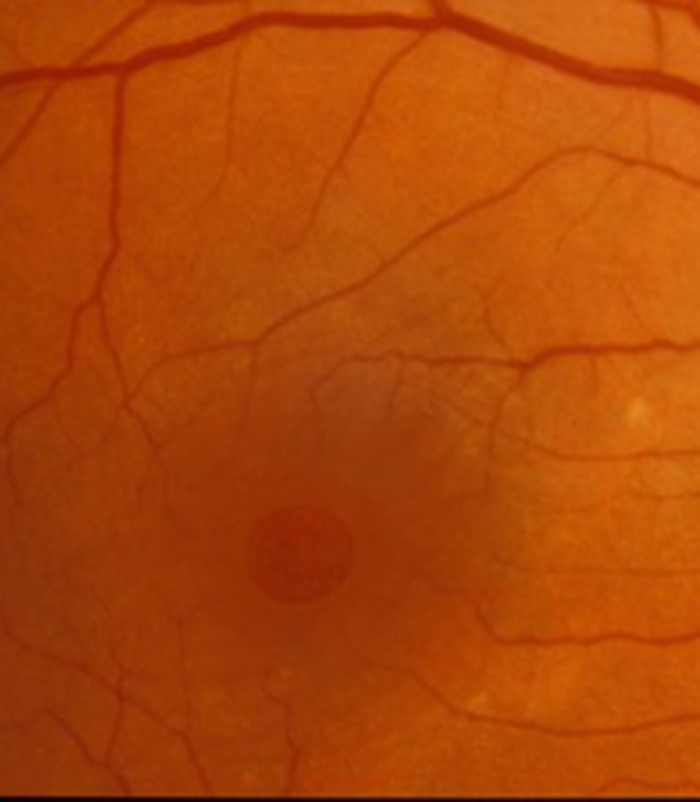
Macular Hole
Mr Simcock has pioneered macular hole surgery in the UK and performs a technique which includes lens removal to prevent patients returning for cataract surgery. The technique also benefits from no or limited (2 day) face down posturing to allow hole closure in most macular holes.

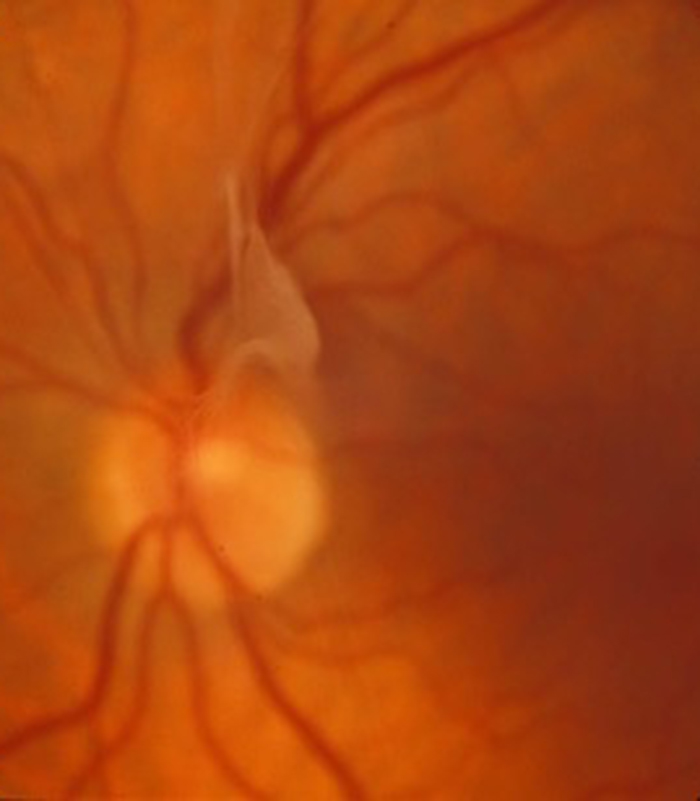
Epiretinal Membrane
Scar tissue on the surface of the macular (central retina) causes blurring and distortion of vision. Surgical removal of scar tissue with vitrectomy can be performed if sufficiently troubled. Most patients notice a significant improvement in vision and reduced distortion with this surgery..
Floaters
Patients troubled by floaters in their vision not improving over a period of at least 6 months may benefit from vitrectomy surgery to remove the floaters. Patient selection is important and depends on age (usually over 50) and the state of the jelly (vitreous) in the main eye cavity.

