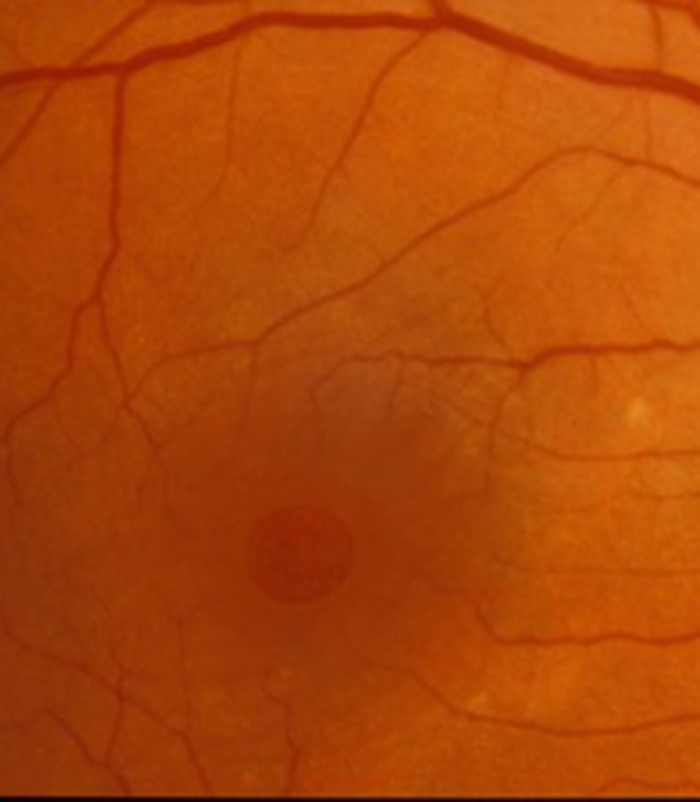
What is a macular hole?
Some patients develop a small hole in the very centre of the retina (photographic film at the back of the eye) called a macular hole. It causes an area of central blurring of vision and sometimes distortion of vision (straight lines becoming kinked or wavy). If left untreated you remain with a blurred patch in the centre of the vision but the peripheral (side) vision remains unaffected. It usually affects one eye only but can affect the second up in up to 10% to 20% of patients.
The eye is like a camera with the lenses at the front and a photographic film (retina) at the back. Between the two in the “body” of the camera is a clear jelly called vitreous. In patients who develop macular hole this jelly pulls on the very centre of the retina and pulls the tissues apart to create the hole. As it is a mechanical or tractional problem that has created the hole, it requires a mechanical or surgical treatment with a procedure called a phacovitrectomy.
What is the surgical treatment of macular hole?
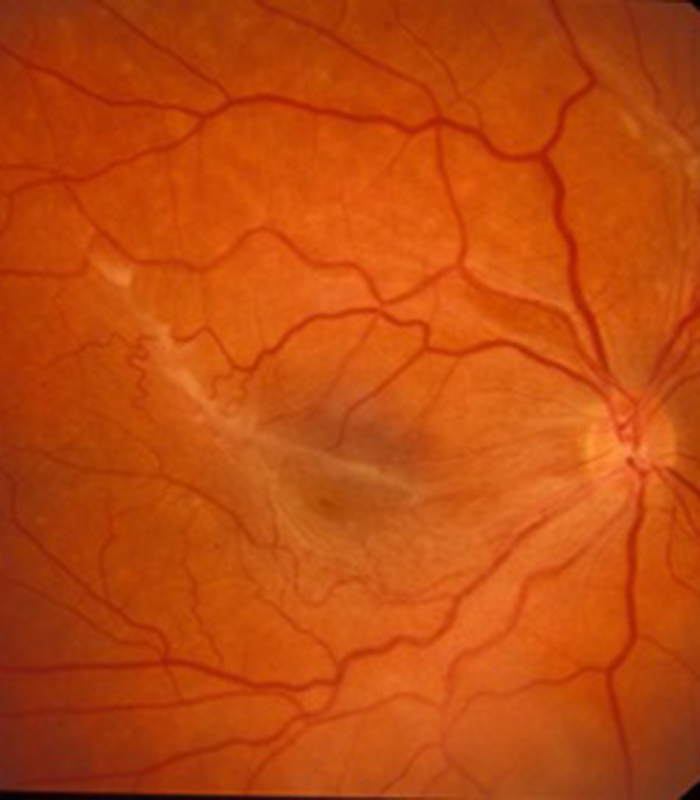
A macular hole develops by the vitreous jelly within the main eye cavity pulling on the central part of the retina and pulling the retinal tissue apart to create a hole. Surgery involves removing this “pulling force” by removing the vitreous jelly from the main eye cavity and replacing it with a “pushing force” to push the tissue together and close the hole. This pushing force is produced by replacing the jelly with a large gas bubble inside the main eye cavity. It was initially thought that in order to “push hard” on the macular hole the patient had to posture “face down” for up to 2 weeks, day and night to allow the gas bubble to float up to the back of the eye to put pressure on the hole.
I performed research in 2000 with a clinical study which was published in the British Journal of Ophthalmology to show that this prolonged posturing was not required in order to produce successful hole closure in most patients. Prolonged posture only needs to be performed in patients with large macular holes of long duration. Most patients with macular holes either need no “face down” posture or only limited posture in this position for the first 24 to 48 hours after surgery. The only restriction in positioning is that patients should avoid lying on their back for the first week following surgery as the gas bubble is least effective in closing the hole in this position as it floats to the front of the eye and away from the macula.
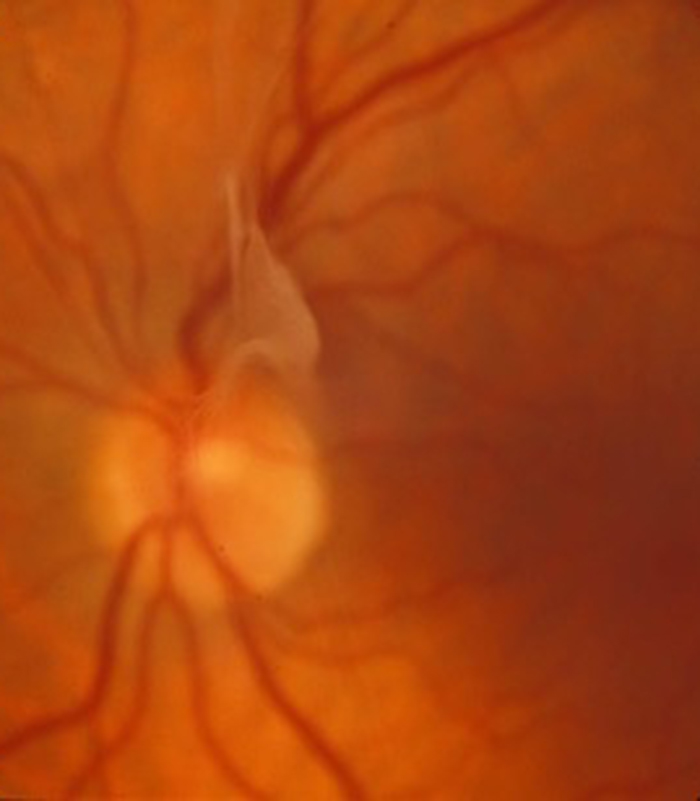
The gas bubble lasts about 6 weeks and gradually gets absorbed back into the blood stream over this period. The eye is initially almost completely full of gas and the vision is very blurred immediately after surgery. As the gas bubble disappears the vision slowly returns. What happens inside the eye is the opposite of what you actually see as things are optically reversed by the eye. Inside the eye the gas is buoyant and floats to the top of the eye when you are in the upright position. As it gets absorbed into the blood stream it is replaced by a clear fluid called aqueous humour which is produced at the front of the eye but following a vitrectomy passes into the vitreous cavity to occupy the whole eye cavity and not just the front of the eye. You first see something at the top of your field of vision and this area of clear vision slowly descends down. Usually by about 3 weeks following surgery you become a “human spirit level” with a “blob” in your vision with the upper half of the vision seeing well and the lower half still being blurred. The vision then continues to improve until usually the bubble breaks up into a few smaller bubbles due to changes in surface tension before they disappear completely. It is advisable not to drive until the gas bubble has completely disappeared and you must certainly not fly. If you significantly increase your altitude (fly or even drive up a high mountain) the gas bubble tries to expand due to the lower pressures in the surrounding atmosphere. Unfortunately because the eye has a rigid corneo-scleral envelope (the strong white of the eye and cornea or clear window at the front of the eye which is attached to the sclera) it cannot expand so as a result the pressure in the eye increases. If the pressure increases to a significant level it cuts off the blood supply to the eye and the vision can be permanently severely damaged. This is why it is so important to not fly until the bubble has completely disappeared. If you have a general anaesthetic for any other condition (such as an emergency operation) whilst there is still some gas in the eye then do please ensure that the anaesthetist knows about your gas bubble as there are certain anaesthetic gases such as nitrous that should not be used because of the same risk of raised pressure inside the eye. You should however have a wrist band placed immediately after your operation stating the gas that has been used. You should keep this wrist band on until the bubble has completely disappeared.
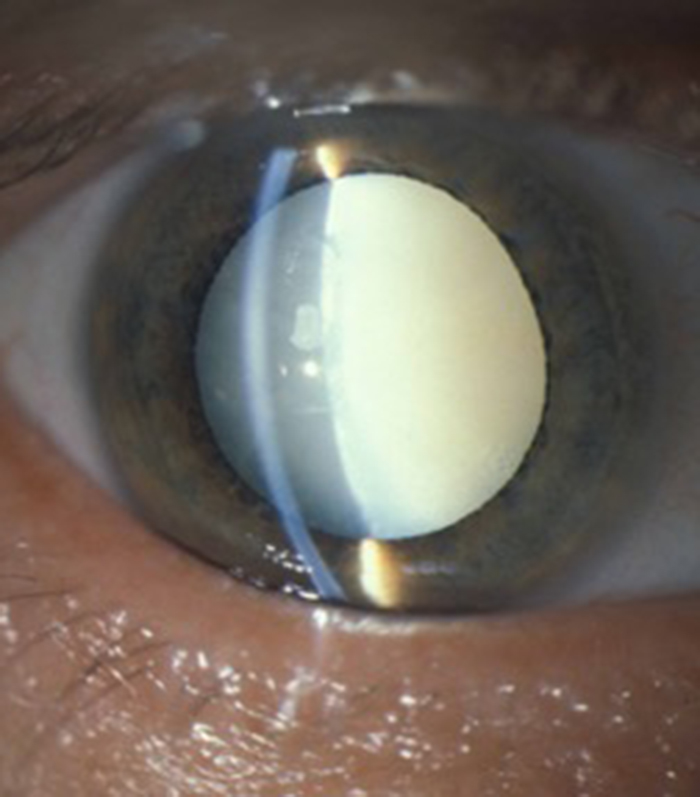
A vitrectomy operation alone will eventually result in the development of cataract and the large gas bubble will also cause progression of cataract. I have been very keen to perform what is called “combined surgery” for patients with macular holes for many years. This involves removing the lens of the eye at the time of the vitrectomy operation and replacing it with a new plastic intra-ocular lens. This is identical to the cataract surgery which occurs when the lens becomes cloudy. The advantage of this “combined” approach is that it prevents you having to come back for further cataract surgery months or years after the vitrectomy operation and also allows a bigger bubble to go inside the eye making face down posturing less necessary.
Surgery for macular hole is under local anaesthetic (usually with some sedation) as a day case procedure. It involves creating three very small incisions in the sclera (white of the eye) at the front of the eye and all instruments are inserted through these small incisions. The operation usually takes about 1 hour. When the combined operation occurs (cataract removal as well as vitrectomy) drops have to be placed onto the eye every 2 hours during the day for the first 2 days then 4 times a day for approximately one month. I normally phone my patients on the first day after surgery and perform a review about 3 weeks after surgery when the gas bubble has shrunk sufficiently to enable a view of the central macula area. An assessment by the optician occurs about 3 months following surgery.
Patients with macular hole complain of blurring and distortion of central vision. The operation has a 9 out of 10 chance of successfully closing the hole. The central retina (macula) is the most sophisticated piece of tissue in the body and it is not surprising that despite successful anatomical closure of the hole it is rare that the vision completely returns to normal. The aim of surgery is to improve rather than cure your symptoms and most patients notice a significant improvement in vision and a reduction in distortion but may be aware of a slight visual disturbance remaining.
Most of the improvement in vision occurs within the first few months following surgery but sometimes things can continue to gradually improve many months after surgery.
Problems we can help with
I will explain with the aid of video clips the various eye problems I treat. This includes cataract surgery, refractive lens exchange in patients over 50 and medical and surgical treatments of all retinal and macular problems.
Cataract
I provides advanced micro-incision cataract surgery and will advise on the appropriate intra-ocular lens for your particular needs. This includes toric lenses to correct astigmatism and extended range of vision multifocal lenses to reduce spectacle dependance.
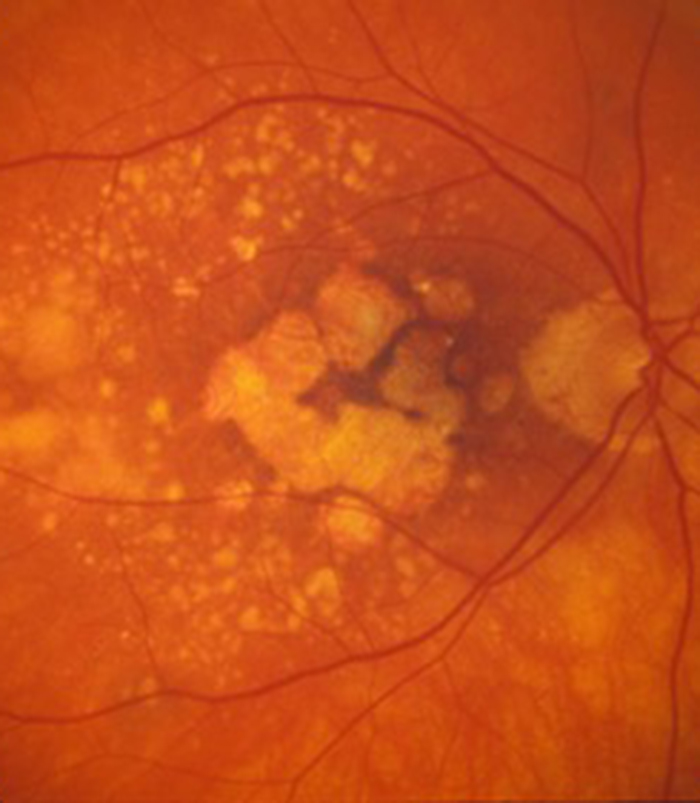
Macular Degeneration
Patients with wet (neovascular) age-related macular degeneration can benefit from prompt injection treatments with various anti-VEGF agents. The first injection can usually be performed on the day of consultation as as "see and treat service".
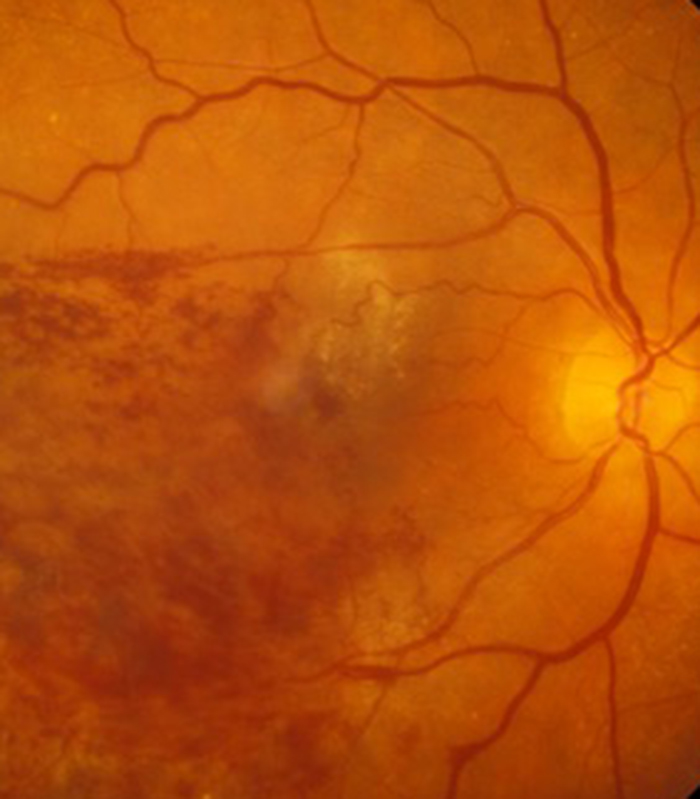
Retinal Vein Occlusion
Blockage to the veins of the retina can produce significant visual disturbance and may require injection treatments with anti-VEGF agents or steroids at Exeter Eye. More severe cases may require laser or surgery at the West of England Eye Unit under Mr Simcock's care..
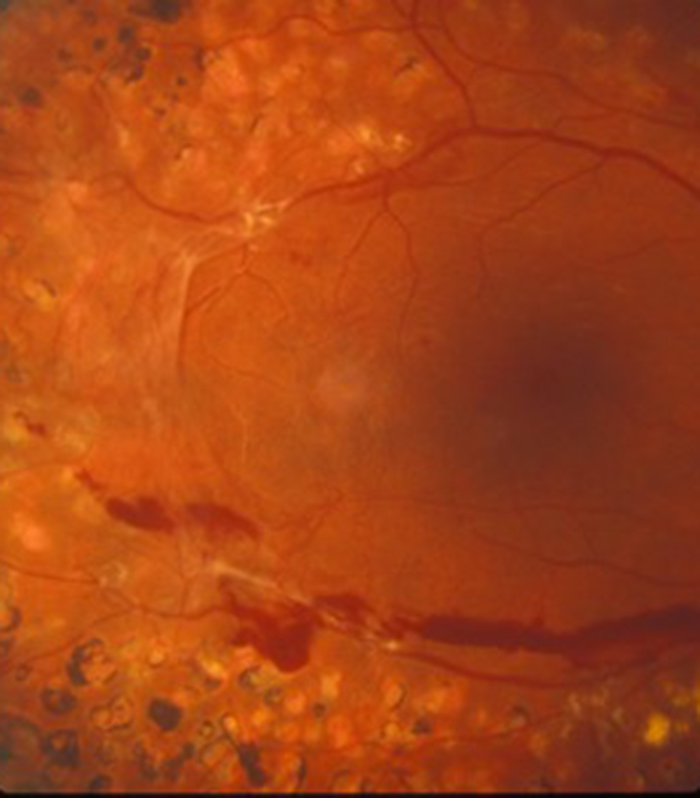
Diabetic Eye Disease
Diabetes is becoming increasingly common and can cause significant visual loss. If detected at an early stage vision can be maintained using injection treatments with anti-VEGF agents or steroids. More serious cases may require laser or surgery at the West of England Eye Unit.
Macular Hole
Mr Simcock has pioneered macular hole surgery in the UK and performs a technique which includes lens removal to prevent patients returning for cataract surgery. The technique also benefits from no or limited (2 day) face down posturing to allow hole closure in most macular holes.
Epiretinal Membrane
Scar tissue on the surface of the macular (central retina) causes blurring and distortion of vision. Surgical removal of scar tissue with vitrectomy can be performed if sufficiently troubled. Most patients notice a significant improvement in vision and reduced distortion with this surgery..
Floaters
Patients troubled by floaters in their vision not improving over a period of at least 6 months may benefit from vitrectomy surgery to remove the floaters. Patient selection is important and depends on age (usually over 50) and the state of the jelly (vitreous) in the main eye cavity.

